TB-Mukt Bharat India's Fight Against Tuberculosis
- 26 Mar 2024
Why is it in the News?
Even though World TB Day (March 24) has passed, recognizing the needs and interests of patients and communities must form the basis of disease elimination.
What is Tuberculosis?
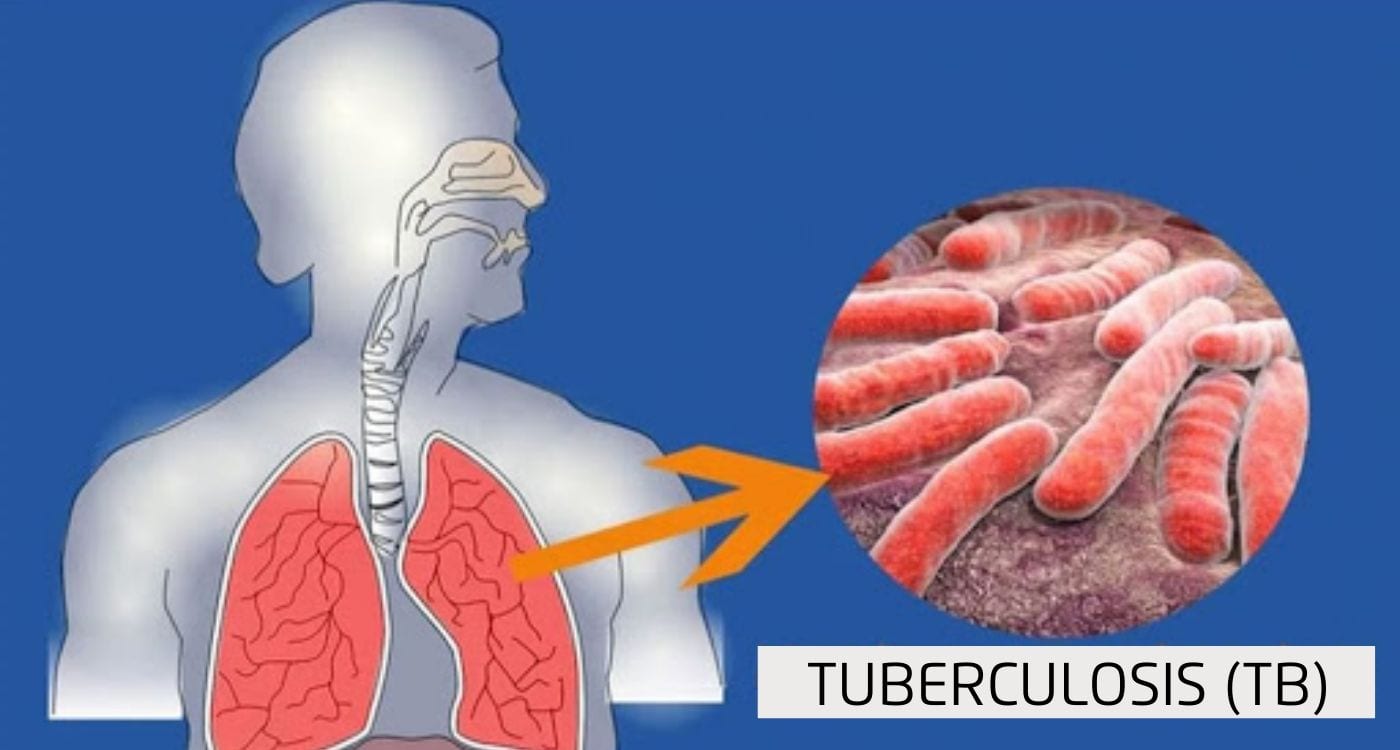
- Tuberculosis (TB) is an airborne bacterial infection caused by a type of bacteria called mycobacterium tuberculosis.
- The infection primarily attacks our lungs and if not treated early, permanent lung damage can result.
- Tuberculosis can also spread to other parts of the body such as the intestines, bones and joints, brain, skin, and other tissues of the body.
- It can be classified into two categories:
- Active tuberculosis (TB) and
- Latent tuberculosis (TB).
Causes of Tuberculosis (TB):
- Mycobacterium tuberculosis usually spreads from person to person through airborne droplets, which are produced when the infected person coughs, sneezes, speaks, or sings.
Signs & symptoms of Tuberculosis (TB):
- A person with latent Tuberculosis (TB) cannot spread the infection to others as it is not contagious and may not show symptoms because their immune system is protecting them from getting sick.
- However, latent TB can develop into active TB if that individual’s immune system cannot stop the bacteria from growing and starts showing symptoms such as:
- Bad cough that lasts for 3 weeks or longer
- Pain in chest
- Coughing blood or sputum
- Fever or night sweats
- Weight loss or no appetite
- Chills
- Weakness
Diagnosis of Tuberculosis (TB):
- Tuberculosis (TB) can be tested in two ways, namely skin test and blood test.
- These two tests only tell if a person has TB or not; if the test is positive then other tests are needed to check if it is latent TB or active TB, such as chest X-ray or CT, or acid-fast bacillus tests (sputum tests).
Treatment of Tuberculosis (TB)
- Both latent TB and active TB can be effectively treated with antibiotics, albeit requiring different durations of treatment.
- Complete adherence to medication is imperative for curing TB; failure to complete the prescribed course may lead to the recurrence of illness and increased difficulty in recovery.
- For latent TB, treatment typically involves a course lasting 3-9 months, comprising 1-2 antibiotics.
- While active TB necessitates a more extensive regimen, with doctors prescribing 2 to 4 or more antibiotics for 6-9 months or longer.
- Ensuring proper medication adherence is crucial for individuals with latent TB to prevent its progression to active TB.
- In many cases, significant improvement is observed within weeks of initiating treatment, with the infection becoming non-contagious.
- Therefore, completing the full course of medication is essential to safeguard oneself and others from tuberculosis.
What is drug-resistant Tuberculosis (TB)?
- Drug-resistant TB is when the bacteria that causes TB becomes resistant to some or all the medications.
- Once drug-resistant TB is developed, it is very difficult to treat it.
- It may require more and different medications with a longer period of treatment.
- Some injectable drugs can cause loss of hearing and balance problems.
Status of TB in India:
- India bears approximately 27% of the global burden of tuberculosis (TB), making it the country with the highest TB burden worldwide.
- Government of India aims to eliminate tuberculosis (TB) by 2025.
- The theme for World Tuberculosis Day (March 24) in 2024 was the same as in 2023 “Yes, we can end TB”, which reflects the United Nations Sustainable Development Goals (SDGs) to eliminate TB by 2030.
Challenges Confronting India in TB Elimination:
- Drug-resistant TB Cases: India grapples with a substantial burden of drug-resistant TB, including multidrug-resistant TB (MDR-TB), necessitating more expensive, specialized drugs and prolonged treatment durations.
- Diagnostics and Case Detection: Accurate and timely TB diagnosis remains a challenge, particularly in areas lacking access to modern diagnostic tools, leading to reliance on older, less reliable methods.
- Poor Primary Healthcare and Infrastructure: Limited access to healthcare facilities, especially in rural and remote regions, results in delayed diagnosis and treatment, facilitating TB transmission within communities.
- Stigma and Awareness: Stigma surrounding TB may deter individuals from seeking timely healthcare, while inadequate awareness about the disease perpetuates its prevalence.
- Private Sector Engagement: With a significant portion of healthcare services provided by the private sector, effective TB control necessitates coordinated efforts and standardized treatment protocols between the public and private sectors.
- Treatment Adherence: Ensuring patient adherence to the full course of TB treatment, which involves prolonged antibiotic courses, poses a significant challenge.
- Vulnerable Populations: Certain demographics, such as migrant workers, urban slum dwellers, and individuals residing in overcrowded conditions, face heightened TB risks, requiring targeted interventions.
Initiatives by the Government of India to Eradicate TB:
- National Tuberculosis Elimination Program (NTEP): A National Strategic Plan (2017-25) aims to eliminate TB from India by 2025.
- Pradhan Mantri TB Mukt Bharat Abhiyan (PMTBMBA): Introduced in 2022, this initiative provides community support to TB patients, offering nutritional, diagnostic, and vocational assistance.
- Revised National Tuberculosis Control Program (RNTCP): Launched in 1997, RNTCP has been continuously revised and strengthened to combat TB effectively.
- Universal Drug Susceptibility Testing (DST): Efforts have been intensified to ensure universal access to drug susceptibility testing, enabling early detection of drug-resistant TB strains for tailored treatment.
- Ni-kshay Portal: An online platform established to monitor notified TB cases effectively.
- Introduction of New Drugs: Drugs like Bedaquiline and Delamanid for treating drug-resistant TB are provided free of cost to TB patients.
- Research and Development (R&D) for Treatment: Studies are ongoing to explore shorter anti-tubercular drug courses, aiming to reduce treatment duration.
- Vaccine Development: Trials are being conducted to evaluate the effectiveness of vaccines such as Immuvac and VPM1002 in preventing TB, offering promising avenues for future TB prevention strategies.
Global Efforts to Eradicate TB:
- End TB Strategy: spearheaded by the World Health Organization (WHO), it provides a roadmap for countries to reduce TB incidence by 80%, and TB deaths by 90%, and eliminate catastrophic costs for TB-affected households by 2030.
- World Development Report (1993): Published by WHO, it highlighted TB treatment for adults as the most cost-effective among all developmental interventions.
- The Global Fund: a global initiative aimed at defeating HIV, TB, and malaria, striving for a healthier, safer, and more equitable future worldwide.
- The Stop TB Partnership: a collaborative effort involving expertise from diverse country, regional, and global partners, dedicated to transforming the TB landscape and achieving the goal of ending TB by 2030.
- Sustainable Development Goal 3: part of the United Nations' Sustainable Development Goals, it targets to end the TB epidemic by 2030, reflecting a commitment to global health and well-being.
Way Forward:
- Development and Widespread Adoption of an Adult TB Vaccine: Prioritizing the research and development of an effective vaccine against TB for adults.
- Ensuring widespread distribution and utilization of the vaccine to bolster TB prevention efforts globally.
- Cost Reduction of Anti-TB Drugs: Implementing strategies to lower the production costs of essential anti-TB medications.
- Making these drugs more accessible and affordable to all individuals in need, regardless of economic status.
- Innovation in TB Treatment: Investing in research and development to create injection-free and orally-administered TB medications.
- Expanding treatment options to enhance patient compliance and improve treatment outcomes.
- Integration of AI-Assisted Radiology: Leveraging artificial intelligence (AI) technology to facilitate rapid and accurate TB diagnosis.
- Promoting the use of handheld radiology devices equipped with AI algorithms, allowing for quick TB detection with high accuracy rates, thereby streamlining diagnostic processes and improving patient care.
