The right to die with dignity
- 26 Oct 2024
In News:
- The Ministry of Health and Family Welfare's draft guidelines (October 2024) aim to implement the Supreme Court's 2018 and 2023 orders on the right to die with dignity.
Legal Context: Supreme Court Rulings and Constitutional Rights
- Right to Refuse Treatment:
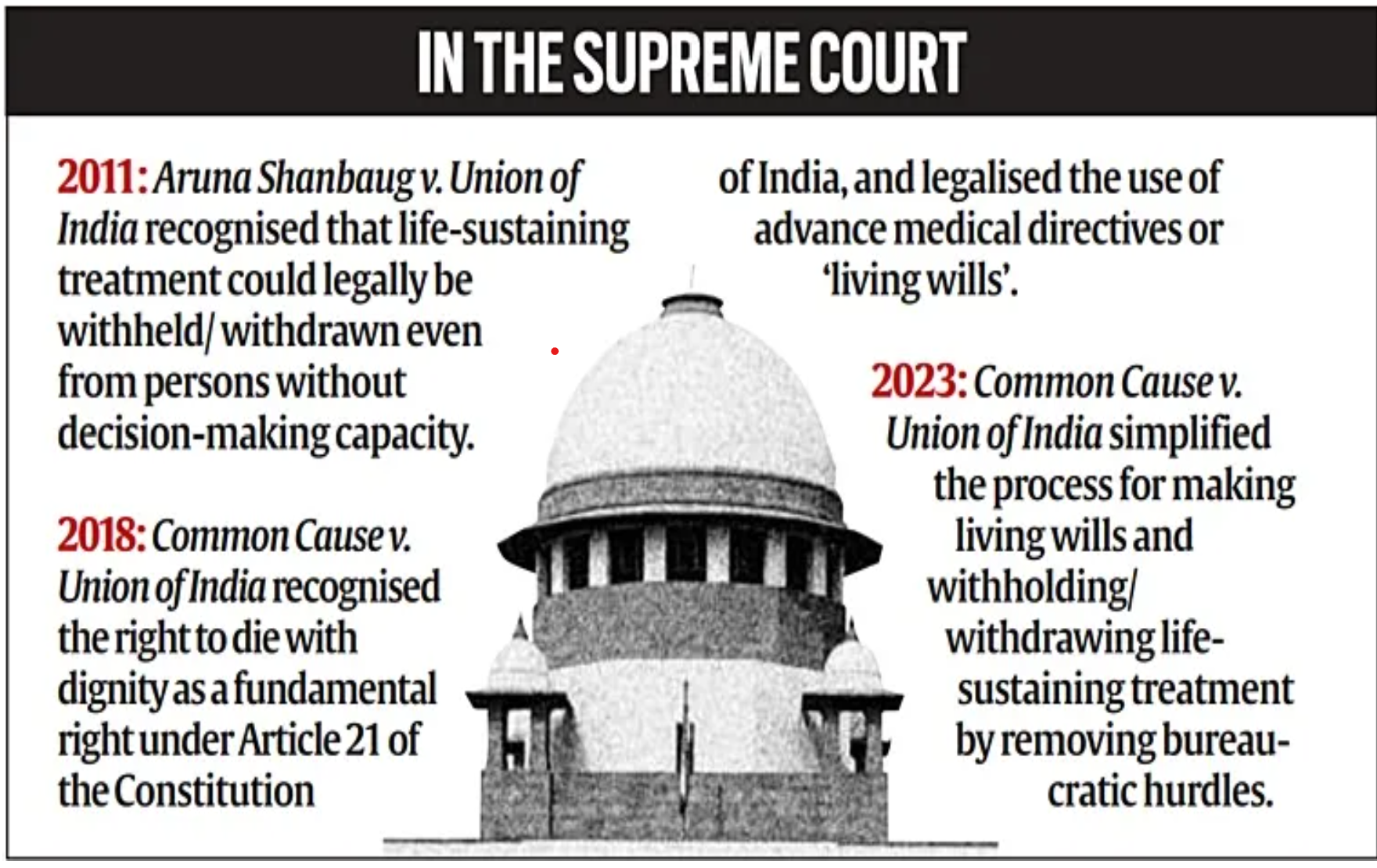
- Common Law & Article 21: The right to refuse medical treatment is grounded in common law and is now recognized as a fundamental right under Article 21 of the Indian Constitution, following the 2018 Supreme Court judgment in Common Cause v. Union of India.
- Supreme Court Rulings: The court's rulings in 2018 and 2023 affirmed that individuals have the constitutional right to refuse life-sustaining treatment and to die with dignity.
Withholding and Withdrawing Life-Sustaining Treatment
- Definition and Meaning:
- What Is Life-Sustaining Treatment? Life-sustaining treatments, such as ventilators and feeding tubes, artificially replace vital bodily functions to sustain life.
- Withholding/Withdrawal: This refers to discontinuing these treatments when they no longer improve the patient's condition or merely prolong suffering.
- When Is It Done?
- End-of-Life Care: Withholding or withdrawing treatment is considered when further medical intervention is futile and would only artificially prolong the dying process.
- Focus on Comfort: After withdrawing life-sustaining measures, the focus shifts to palliative care to alleviate pain and suffering.
Understanding Euthanasia and Misconceptions
- What Is Euthanasia?
- Definition: Euthanasia refers to the intentional ending of a terminally ill patient’s life by medical professionals to relieve suffering.
- Passive Euthanasia Misconception: In India, the term "passive euthanasia" is often mistakenly used to describe withholding or withdrawing life-sustaining treatment, but this does not involve the active killing of the patient.
- Legal Framework: The Indian Council of Medical Research (ICMR) clarified in 2018 that "passive euthanasia" is not a legally accepted practice in the country.
The Role of Doctors: Ethical Dilemmas and Shared Decision-Making
- Is Withdrawing Treatment "Giving Up" on the Patient?
- Not Abandonment: Withdrawing life-sustaining treatment is not about abandoning the patient but recognizing when further interventions would cause unnecessary suffering.
- Palliative Care: The patient’s comfort and dignity are prioritized through palliative care, which focuses on pain management and emotional support for both the patient and family.
- Doctors' Ethical Responsibility:
- Shared Decision-Making: The process encourages a collaborative approach between doctors and the patient’s family or surrogate decision-makers. This joint decision-making ensures that the wishes of the patient are respected and relieves the doctor from bearing sole responsibility for life-and-death decisions.
Living Wills and Advance Medical Directives
- What Is a Living Will?
- Definition: A living will is a legal document where a person outlines their medical preferences in the event they lose decision-making capacity.
- Eligibility and Process: Individuals aged 18 or older, who are capable of making decisions, can draft a living will, naming at least two trusted surrogate decision-makers.
- Legal Requirements: The document must be signed in the presence of an executor, two witnesses, and notarized to be legally binding.
- 2023 Supreme Court Guidelines: The Court simplified the procedure for making living wills to ensure that the right to die with dignity is upheld.
Medical Procedure for Withholding or Withdrawing Treatment
- Supreme Court Guidelines
- The Supreme Court laid out a clear procedure for withholding or withdrawing life-sustaining treatment, emphasizing patient autonomy, expert assessments, and family consent.
- Primary and Secondary Medical Boards:
- Primary Medical Board: The treating hospital sets up a Primary Medical Board, consisting of the treating doctor and two subject-matter experts, to assess the patient's condition and determine if life-sustaining treatment is appropriate.
- Secondary Medical Board: A Secondary Medical Board, comprising independent experts, reviews the Primary Board's decision for added oversight.
- Consent from Family/Surrogate Decision-Makers:
- The patient’s wishes, as outlined in an advance directive or by a surrogate, must be respected, and their consent is essential for proceeding with treatment withdrawal.
- Judicial Oversight:
- Once the decision to withdraw treatment is made, the hospital is required to notify the local judicial magistrate, ensuring transparency and accountability.
Conclusion: Legal and Ethical Clarity in End-of-Life Care
- Shared Decision-Making: The process ensures that medical teams, families, and surrogate decision-makers collaborate, preventing any medical professional from facing moral or legal dilemmas alone.
- Protection of Autonomy: These frameworks and guidelines uphold patient autonomy, offering a legal and ethical pathway for terminally ill patients to exercise their right to die with dignity.
