Biomedical Waste Regulations

- 30 Nov 2024
The Emergence of HIV and Global Panic
In 1983, scientists Luc Montagnier and Robert Gallo independently identified the virus responsible for AIDS. By the mid-1980s, HIV/AIDS was perceived as a biological death sentence, with the virus primarily attacking immune cells, making medical intervention difficult. The epidemic quickly became associated with fear, ignorance, and stigma, as it was often linked to marginalized groups.
The "Syringe Tide" Incident and Public Outrage
In August 1987, the U.S. faced a public health crisis when discarded medical waste, including syringes and blood vials, washed up on beaches along the Atlantic coast. Known as the "Syringe Tide," this incident shocked the public and fueled anxiety, especially when children were seen playing with syringes. Traced to improper waste disposal in New York City, the event highlighted the hazardous nature of medical waste, which had been previously underestimated. Combined with the HIV/AIDS epidemic, this incident amplified public fear and economic losses of up to $7.7 billion due to the decline in tourism.
U.S. Response: Medical Waste Tracking Act of 1988
The widespread outrage led to the U.S. government passing the Medical Waste Tracking Act in 1988. This was the first law to formally categorize hospital waste as hazardous. The Act introduced stringent guidelines for the handling, transportation, and disposal of medical waste, establishing systemic regulation and oversight. It marked a significant turning point in both public health and environmental safety, changing how medical waste was managed in the healthcare sector.
India’s Journey in Biomedical Waste Management
Initial Steps and Delays
While the U.S. responded swiftly to the crisis, India’s approach to managing biomedical waste was slower. In 1986, India enacted the Environmental Protection Act, which marked the country’s first significant step towards environmental conservation. That same year, India identified its first HIV case. However, biomedical waste was not yet recognized as hazardous, and the Hazardous Waste (Management and Handling) Rules of 1989 failed to address the issue. As a result, local bodies were left to manage waste disposal, leading to inefficiencies.
Judicial Intervention and Legislative Action
In the 1990s, as pollution levels rose, particularly in urban areas like Delhi, the inadequacies of the system became apparent. In the landmark case Dr. B.L. Wadehra vs. Union of India (1996), the Supreme Court criticized Delhi’s waste management system, calling the city an "open garbage dump." This judgment led to a nationwide conversation on waste management and resulted in the Biomedical Waste (Management and Handling) Rules of 1998, marking the formal recognition of hospital waste as hazardous. The rules empowered the Central and State Pollution Control Boards to regulate waste disposal, ensuring accountability.
The Link Between HIV and Biomedical Waste Regulations
The HIV crisis highlighted the need for safe disposal practices to protect the environment and healthcare workers. While India charted its own course, the global response to HIV, particularly the U.S. model, influenced India’s approach to biomedical waste management. Over the years, India has made significant progress, with amendments to the rules in 2016 and 2020 to improve waste management technology and ensure safe disposal.
Current Challenges and Progress
- Ongoing Issues in Biomedical Waste Management: Despite significant progress, challenges remain, especially in rural and resource-limited areas. Mishandling of biomedical waste continues to pose risks, and healthcare professionals still face occupational hazards. Gaps in compliance and awareness persist, but the system’s progress is undeniable.
Conclusion
The HIV/AIDS epidemic, while tragic, indirectly led to significant improvements in healthcare waste management. As the crisis highlighted the dangers of improper waste disposal, it spurred legislative and systemic changes that have contributed to safer healthcare environments. The progress in biomedical waste management demonstrates that crises can often lead to long-term improvements.
The Mental Health Crisis in India

- 10 Oct 2024
In News:
India faces a significant mental health crisis, driven by various factors including economic disparities, social isolation, and changing family dynamics. The pandemic further worsened these issues, leading to detrimental effects on mental well-being.
Causes of Mental Illness
- Socioeconomic Factors: Poverty, violence, inequality, and environmental deprivation contribute to rising mental health issues.
- Pandemic Impact: Lockdowns and uncertainties have heightened stress levels and anxiety.
- Adverse Life Experiences: Trauma, abuse, and dysfunctional family relationships can severely impact mental health.
- Cultural Pressures: The urban focus on consumerism and status can lead to feelings of inadequacy and dissatisfaction.
The Shortage of Mental Health Professionals
India's mental health services are severely lacking, with only 0.75 psychiatrists per 100,000 population—far below the World Health Organization's recommendation of three. This shortage underscores the need for policy interventions and incentives to increase the supply of mental health professionals.
Government Initiatives for Mental Health
The Indian government has implemented several initiatives to improve mental health care:
- National Mental Health Programme (NMHP): Launched in 1982 to enhance community-based mental health services.
- Mental Healthcare Act, 2017: Decriminalized suicide attempts and introduced advanced directives for treatment choices.
- Rights of Persons with Disabilities Act, 2017: Recognizes mental illness as a disability, enhancing rights for affected individuals.
- Manodarpan Initiative: Provides psycho-social support to students.
- Kiran Helpline: A suicide prevention helpline for crisis management.
- National Tele-Mental Health Programme: Launched in 2022 to expand access to mental health services, particularly in underserved areas.
Economic Survey 2023-24
For the first time, the Economic Survey emphasized the importance of mental health in policy recommendations, calling for effective implementation of mental health initiatives to address existing gaps.
Understanding Healthy Workplaces
Defining a Healthy Workplace
A healthy workplace fosters collaboration between employers and employees to promote physical and psychological safety. It encompasses open communication, respect, and a supportive environment, crucial for addressing workplace stress, anxiety, and burnout.
Current Crisis: Overwork and Mental Health
The phenomenon of ‘Karoshi’ (death from overwork) highlights the severe consequences of workplace stress. In India, 40% of employees report high stress levels due to excessive work demands.
Ethical Perspectives on Healthy Workplaces
Creating a healthy workplace involves:
- Fairness and Equity: Ensuring all employees have equal access to resources and opportunities.
- Respect for Individual Dignity: Acknowledging contributions and fostering psychological safety.
- Moral Responsibility of Employers: Providing a safe working environment and promoting mental health initiatives.
- Transparency and Accountability: Building trust through open communication about policies and practices.
- Promoting Work-Life Balance: Encouraging a balance between professional and personal life to prevent burnout.
Global Precedents for Work-Life Balance
Countries like Australia and France have introduced regulations, such as the ‘right to disconnect,’ allowing employees to disengage from work communications after hours.
Conclusion and Way Forward
Establishing healthy workplaces is not merely a regulatory compliance issue but an ethical commitment to employee well-being. Both employers and employees must collaborate to create an environment of psychological safety, open communication, and mutual respect. By prioritizing these principles, organizations can foster workplaces that enhance productivity and support mental health, ultimately driving innovation and improving overall well-being.
The Path to Universal Health Coverage: Embracing Data and Digital Technology

- 13 Sep 2024
The expansion of Universal Health Coverage (UHC) represents a complex but crucial endeavor. The integration of data and digital technology stands out as a pivotal factor in smoothing the way towards achieving this goal.
Understanding Universal Health Coverage
Universal Health Coverage means ensuring that every individual has access to the full spectrum of quality health services when and where they need them, without facing financial hardship. This concept encompasses a broad range of essential health services, including health promotion, prevention, treatment, rehabilitation, and palliative care throughout an individual's life.
UHC as a Sustainable Development Goal
Achieving UHC is a key target of the Sustainable Development Goals (SDGs) established by the global community in 2015. However, despite this commitment, progress towards this goal remains off-track. Since 2015, improvements in health services coverage have stalled, and the proportion of people facing catastrophic out-of-pocket health expenses has been rising steadily since 2000.
Challenges to Universal Health Coverage
Several challenges hinder the advancement of UHC:
- Global Stagnation: Progress in health coverage has stagnated globally, affecting regions and countries alike.
- Manpower Shortages: Many Western and Central Asian countries face severe healthcare manpower shortages.
- Pandemic Disruptions: The COVID-19 pandemic has further disrupted essential health services, with 92% of countries experiencing interruptions at the pandemic's peak in 2021, and 84% still reporting disruptions in 2022.
- Inequality in Healthcare Spending: The disparity between poor and non-poor households has widened, with lower-income families often forced to deplete their resources or sell assets to cover healthcare costs. According to the WHO, 55 million people fall into poverty annually due to catastrophic health expenditures.
- Insufficient Spending: India’s healthcare spending, currently at 3.2% of its GDP, is lower than the average spending of 5.2% observed in lower and middle-income countries (LMICs). The government’s health expenditure is also lower compared to other countries like China, Thailand, Vietnam, and Sri Lanka.
Opportunities Through Digital Health
To address these challenges, leveraging digital health solutions is critical. India's leadership in digital health is exemplified by the Global Initiative on Digital Health, launched under India’s G20 presidency. This initiative aims to drive investments into digital health and facilitate regional and international collaboration.
India’s Ayushman Bharat Digital Mission, which precedes this global initiative, highlights the country's commitment to using digital technology to manage the complexities of UHC expansion. Digital health tools can play a transformative role in managing contracts, implementing value-based provider reimbursements, and streamlining healthcare delivery.
The Role of Artificial Intelligence
Artificial Intelligence (AI) holds significant promise for revolutionizing healthcare. AI-powered diagnostic tools can improve the accuracy and speed of medical diagnoses, leading to better patient outcomes. AI can also predict disease outbreaks, analyze healthcare data, optimize treatment plans, and enhance drug discovery, making healthcare more personalized and effective.
Building Digital Infrastructure
India’s experience in expanding digital health infrastructure can serve as a model for other low- and middle-income countries. Many of these nations are seeking to build and enhance their healthcare systems, and India’s approach may offer valuable policy insights.
The Need for Private Sector Participation
Achieving UHC in India cannot rely solely on the public sector. Integrating the private sector into the public healthcare framework is essential. Addressing modern health challenges requires a collaborative effort that includes both public and private sectors, creating a multifaceted and synergistic approach to healthcare.
WHO’s Recommendations
To strengthen health systems, the WHO recommends reorienting them with a primary health care (PHC) approach. Implementing PHC can deliver up to 90% of essential UHC interventions, potentially saving 60 million lives and increasing global life expectancy by 3.7 years by 2030.
Looking Ahead
It is crucial to balance national interests with international ambitions and leverage digital technologies to create inclusive solutions. Countries should build on their existing systems, gradually implementing reforms and best practices. With dedicated effort and a commitment to excellence, it is possible to build a healthier and more prosperous future for generations to come.
India’s sickle cell challenge
- 12 Sep 2024
In News:
Last year, Prime Minister Narendra Modi launched the National Sickle Cell Anaemia Elimination Mission to eliminate sickle cell disease as a public health problem by 2047, from Shahdol, Madhya Pradesh.
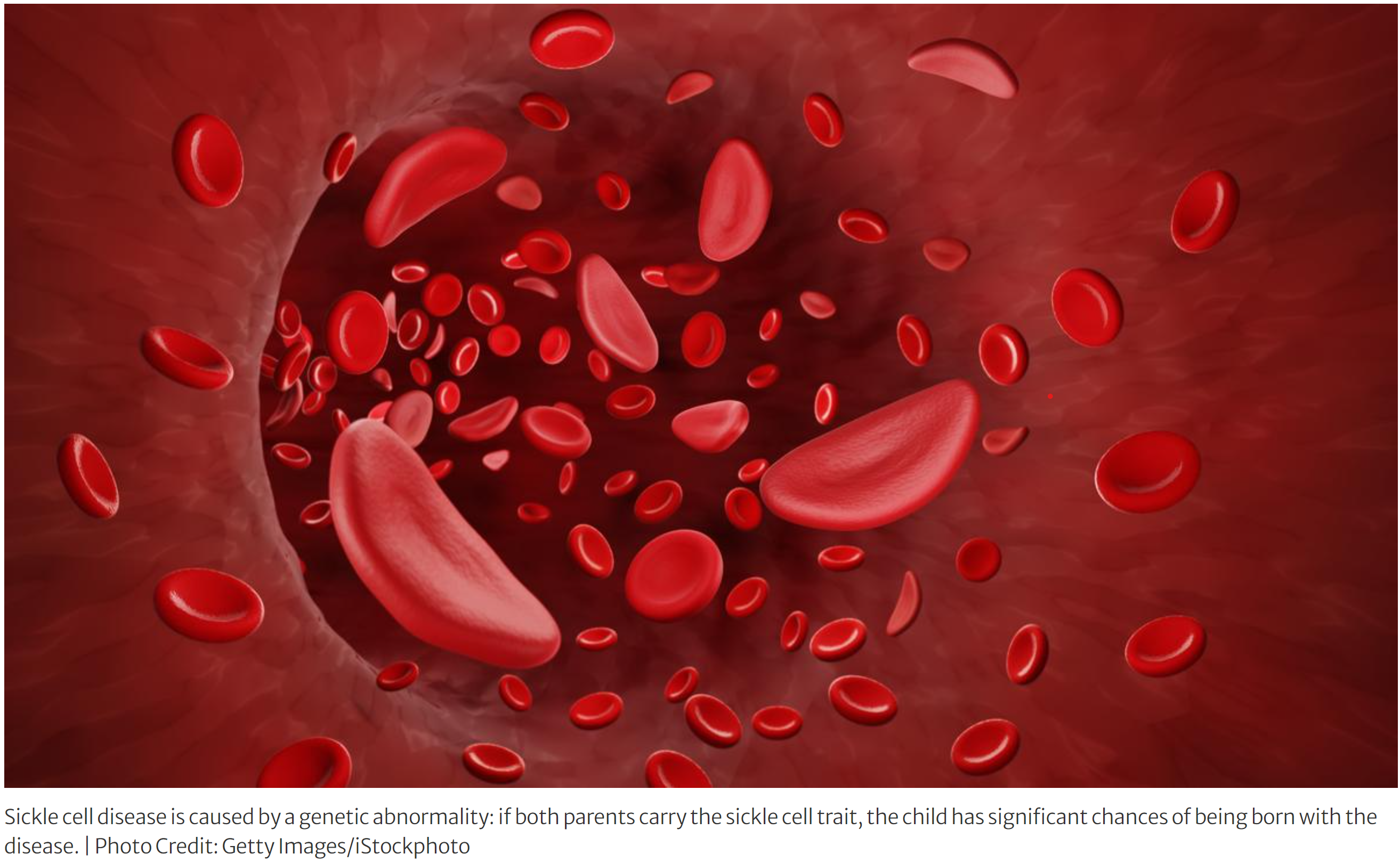
What is Sickle Cell Disease?
- It is a genetic blood disorder that affects the shape of red blood cells. Normally, red blood cells are round and flexible, but in sickle cell disease, they become stiff and crescent-shaped, resembling a sickle.
- This abnormal shape makes it difficult for these cells to travel smoothly through blood vessels, leading to blockages and various health problems.
- It is caused by a mutation in the gene that tells the body how to make hemoglobin, the protein in red blood cells that carries oxygen.
- Both parents must pass down the defective gene for a child to develop the disease.
- If a person inherits the gene from just one parent, they have sickle cell trait and can pass the gene to their children but usually do not experience symptoms.
- Symptoms:
- Episodes of severe pain, called pain crises, typically in the chest, joints, and bones.
- Fatigue and anemia, due to the rapid breakdown of red blood cells.
- Swelling in the hands and feet, caused by the sickle-shaped cells blocking blood flow.
- Frequent infections, as the spleen, which helps fight infection, may be damaged by the disease.
- Delayed growth and puberty in children, due to chronic anemia.
- Diagnosis:
- It is usually diagnosed through a blood test. Newborns are routinely screened for the disease in many countries.
- The test checks for the presence of hemoglobin S, the defective form of hemoglobin that causes sickle cell disease.
- Treatment:
- While there is no universal cure for sickle cell disease, treatments can help manage symptoms and reduce complications.
- Pain relief medications for pain crises.
- Blood transfusions to treat anemia and prevent stroke.
- Hydroxyurea, a medication that can reduce the frequency of pain crises and the need for blood transfusions.
- Bone marrow or stem cell transplants, which can potentially cure the disease but are not suitable for all patients due to risks and availability of donors.
- Challenges in India
- India, with over a million affected individuals, faces the world’s second largest burden of sickle cell disease, primarily affecting tribal regions across Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh, and Maharashtra. Only 18% of those affected receive consistent treatment due to significant drop-offs at diagnosis and adherence stages. Diagnosis is hindered by stigma and reliance on traditional healers, with a lack of trust in the public healthcare system. Treatment adherence is also poor due to the absence of a permanent cure, inadequate supply of essential medications like hydroxyurea, and logistical challenges, including long travel distances for medicine. Additionally, vaccination coverage, which helps improve patients' quality of life, remains insufficient.
The way ahead
- It is important to reduce the stigma related to the disease and build trust in public health institutions. Awareness should be raised through targeted media campaigns to bust specific myths (which vary by region and tribe).
- Second, given that cases are often missed and diagnosis delayed, there could be increasing screening for newborns. This strategy is low-cost with a high pay-off and would especially be effective in areas where the condition is endemic.
- Third, drugs as well as adherence support must be available close to patients, in the nearest health and wellness centres. For complications, interdisciplinary centres of excellence at the district/division levels should be made operational.
- Fourth, ensuring that all known patients receive approved vaccines will be crucial; this may require catch-up vaccination programmes.
- Fifth, health in tribal areas should be operationally strengthened by factoring in conditions unique to these areas. Healthcare should also be adequately funded.
- Finally, research should be conducted to better understand the disease and its pathways in India, and to develop new treatments. Philanthropists and members of civil society must play a catalytic role, and work with the Central and State governments.
Restoring Earth’s Right to ‘Good Health’

- 23 Apr 2024
Why is it in the News?
The European Court of Human Rights found Switzerland guilty of violating the rights of women from KlimaSeniorinnen, stating that the government's emission control efforts were insufficient, failing to protect women from climate change impacts.
Context:
- Courts worldwide are increasingly tasked with addressing the nexus between climate change and human rights, as evidenced by significant rulings such as those from the European Court of Human Rights in Switzerland and the Supreme Court of India.
- These landmark decisions highlight the imperative of acknowledging climate change as a human rights issue and establishing crucial benchmarks for legal and policy responses to mitigate its detrimental effects on people and societies.
Legal Acknowledgment of Climate Change's Human Rights Impacts:
- Recent rulings by the European Court of Human Rights against the Government of Switzerland and the Supreme Court of India have underscored the failure to safeguard vulnerable populations from the effects of climate change.
- The European Court's decision highlighted the government's neglect in protecting elderly women from climate-related harm, while the Indian Supreme Court affirmed citizens' entitlement to freedom from adverse climate effects under constitutional guarantees.
- Citing Articles 14 (equality before the law) and 21 (right to life and personal liberty) of the Indian Constitution, the Supreme Court emphasized individuals' right 'to be free from the adverse impacts of climate change.'
- These legal judgments signify a significant step towards acknowledging climate change as a pivotal human rights concern.
The Escalating Human Rights Risks of the Global Climate Crisis:
- The global climate crisis presents an imminent threat to human rights, imperiling individuals and communities worldwide.
- The latest State of the Global Climate Report from the World Meteorological Organization presents compelling evidence of the intensifying impacts of climate change.
- In 2023, numerous climate indicators soared to unprecedented levels, marking it as the hottest year on record.
- This unparalleled warmth coincided with concerning trends such as heightened ocean heat accumulation, rising sea levels, diminishing Antarctic sea ice, and accelerated glacier retreat.
- These indicators underscore the severe strain on our planet, with profound implications for human welfare.
India's Climate Action and Vulnerability:
- Progress Amid Persistent Vulnerability: Despite notable advancements in climate action, India, among the world's fastest-growing economies, continues to confront significant vulnerability to climate change.
- Having met two of its Nationally Determined Contribution (NDC) targets—reducing emissions intensity by 33% to 35% and achieving 40% cumulative non-fossil fuel electricity capacity—well ahead of schedule, India demonstrates proactive measures.
- Nevertheless, the nation remains highly susceptible to climate-related adversities.
- Population Concentration in Disaster-Prone Areas: A primary concern is India's demographic distribution, with over 80% of its populace residing in regions prone to climate-induced calamities like floods, cyclones, droughts, and heatwaves.
- These events not only disrupt lives but also exacerbate existing socio-economic disparities, disproportionately impacting vulnerable groups such as small-scale farmers, rural communities, and marginalized populations.
- Intersecting Challenges of Climate Change: Climate change intersects with broader socio-economic and environmental issues, compounding their repercussions.
- Rapid urbanization and haphazard development intensify urban vulnerability to climate-driven disasters like flooding and landslides.
Frameworks to Strengthen India's Climate Action:
- Embracing Comprehensive Legislation: India's climate governance could benefit from the adoption of a comprehensive regulatory framework dedicated to climate change.
- This legislation would offer a unified structure for addressing diverse climate-related aspects, spanning mitigation, adaptation, finance, and capacity-building.
- By enshrining climate objectives, targets, and strategies in law, such a framework can furnish legal clarity and consistency, guiding sustained planning and investment.
- Insights from Global Climate Laws: Research from the London School of Economics and Political Science examined climate framework laws in 60 nations, spotlighting their pivotal role in shaping national climate agendas.
- Countries like Germany, Ireland, New Zealand, Finland, South Korea, South Africa, and the Philippines have instituted robust climate legislation surpassing mere compliance with international obligations.
- These laws have facilitated public resource mobilization, bolstered climate action capabilities, and fostered inter-sectoral cooperation.
Additional Measures for Enhanced Climate Governance in India:
- Integrated Climate Policies: India's climate strategies should embrace an integrated approach, embedding climate considerations into broader development frameworks and decision-making processes.
- This entails weaving climate adaptation and mitigation efforts throughout key sectors like agriculture, water management, energy, transportation, and urban development to foster a cohesive response to climate challenges.
- Localized Solutions and Cross-Sector Collaboration: Tailored, localized climate actions, coupled with collaborative efforts across sectors, are vital for addressing the diverse and context-specific impacts of climate change.
- Governments can craft targeted strategies to bolster resilience, mitigate risks, and advance sustainable development goals by engaging local stakeholders and fostering partnerships across sectors.
- Harmonizing Climate and Sustainable Development Goals: Localized climate initiatives often align with broader Sustainable Development Goals (SDGs), such as poverty eradication, food security, access to clean water, and gender equity.
- Integrating climate considerations into local SDG agendas enables governments to leverage synergies, optimize resource use, and fortify community resilience and sustainability.
- Empowerment of Civil Society: Civil society organizations (CSOs) play a pivotal role in advocating for climate action, environmental equity, and governmental accountability.
- Empowering CSOs and fostering rights-based discourse on climate change are vital for fostering inclusive decision-making, transparency, and environmental justice.
- Fostering Inclusivity and Representation: Promoting diversity and inclusivity within civil society is imperative to ensure the voices and perspectives of marginalized communities are heard and heeded in climate policymaking.
- CSOs should aim to represent the interests of various stakeholders, including women, indigenous populations, youth, persons with disabilities, and other marginalized groups, in climate governance.
- Advancing Rights-Centric Discourse: A rights-based approach to climate action acknowledges that climate change disproportionately impacts vulnerable communities, infringing upon their basic human rights to life, health, food, water, and livelihoods.
- By framing climate change as a human rights issue, CSOs can advocate for policies that prioritize the needs of affected communities and champion environmental justice.
Conclusion
The alignment of legal rulings, scientific findings, and policy mandates emphasizes the pressing imperative to confront climate change as a human rights emergency.
By acknowledging the inseparable link between environmental health and human welfare, nations can pave the way toward climate resilience and equity.
Empowering communities, fortifying legal structures, and promoting cross-sectoral cooperation stand as pivotal measures in realizing a future liberated from the detrimental effects of climate change.
Legal Amendments Likely to Increase Medicine Costs without Improving Quality

- 22 Apr 2024
Why is it in the News?
The amended rules will prolong the life of drugs on account of frivolous patenting, increase their prices, and make lives difficult for patients.
Context:
- India's healthcare system depends largely on accessible medications, with the generic pharmaceutical sector crucial for delivering quality drugs at affordable rates.
- The expense of medicines represents a substantial part of healthcare spending, with almost half of individuals' medical costs dedicated to purchasing prescriptions.
- Yet, the considerable expenses associated with medications, largely influenced by patenting, create significant hurdles for obtaining vital treatments.
What is the Role of Generic Pharmaceutical Companies?
- Generic pharmaceutical companies are pivotal in addressing the challenge of affordability by offering cost-effective alternatives to patented drugs.
- India's generic industry has earned global recognition for its role in providing essential medications at accessible prices.
- The development of India's patent laws has significantly influenced its pharmaceutical sector and its capacity to produce generic drugs.
- Initially, the Indian Patent Act of the early 1970s limited patent protection to the manufacturing processes rather than the products themselves.
- This approach facilitated the growth of the generic industry, positioning India as a major exporter of generic drugs by the late 1980s.
- However, recent revisions to the Indian Patent Law pose a threat to this ecosystem and jeopardize access to affordable healthcare.
What is the Impact of the TRIPS Agreement on India's Pharmaceutical Industry?
- The Trade-Related Aspects of Intellectual Property Rights (TRIPS) Agreement, introduced in 1995, had a significant impact on India's pharmaceutical sector, shaping its development and global position. Key aspects of this impact include:
- Transition to Product Patents: A critical change brought by TRIPS was the requirement for member countries to grant patents for both products and processes, including pharmaceuticals.
- This shift from process to product patents posed challenges for India's thriving generic pharmaceutical industry, which had previously capitalized on producing affordable versions of patented drugs.
- Challenges for India's Generic Industry: The introduction of product patents threatened India's generic pharmaceutical sector, renowned for its capacity to manufacture low-cost essential medicines.
- These patents granted exclusive rights to inventors, restricting generic manufacturers' ability to produce and distribute affordable alternatives.
- Pressure to Comply with International Standards: The TRIPS Agreement pressured India to align its intellectual property laws with international standards, encompassing pharmaceutical patent protection.
- This necessitated amendments to India's Patent Act to comply with TRIPS obligations while preserving the interests of its generic pharmaceutical industry and public health priorities.
- Preserving Access to Medicines: Despite TRIPS challenges, India implemented measures to safeguard access to affordable medicines.
- Provisions like Section 3(d) of the Indian Patent Act, introduced in 2005, aimed to prevent granting frivolous patents for incremental innovations lacking significant therapeutic benefits.
- This ensured compliance with TRIPS requirements while maintaining access to affordable medicines.
- Balancing Innovation and Access: The TRIPS Agreement presented India with the challenge of balancing innovation and access to essential medicines.
- While patents incentivize innovation and investment in research and development, they can restrict access to life-saving treatments, particularly in developing countries with limited healthcare resources.
- Global Leadership in Generic Manufacturing: Despite the challenges posed by TRIPS, India emerged as a global leader in generic drug manufacturing.
- Leveraging its manufacturing capabilities and adherence to TRIPS flexibilities, the country's generic pharmaceutical industry continued to thrive, supplying affordable medicines domestically and globally.
What is Section 3(d) of India's Patent Act?
- Section 3(d) is a crucial provision in India's Patent Act that exemplifies the flexibilities embedded within the country's patent laws.
- It tackles concerns related to "evergreening"—a practice used by pharmaceutical companies to extend patent life through minor modifications or incremental innovations.
- The primary objective of Section 3(d) is to prevent the granting of patents for incremental innovations that lack significant therapeutic efficacy or novelty.
- By doing so, it aims to protect access to generic versions of essential medicines and promote affordability.
- Under Section 3(d), pharmaceuticals and chemical substances are eligible for patent protection only if they demonstrate enhanced efficacy compared to existing formulations.
- This requirement ensures that patents are granted for inventions representing genuine advancements in therapeutic efficacy rather than minor modifications or variations of existing drugs.
- Through Section 3(d), India's patent laws strike a balance between innovation and public health priorities, contributing to the overall well-being and access to medicines for its citizens.
What are the Contemporary Challenges in India's Patent Regime?
- India's patent regime currently faces several challenges, including issues related to pre-grant opposition, competition, international trade agreements, and flexibilities in patent law. These challenges have implications for access to affordable medicines, the financial burden on patent opponents, and drug availability.
- Threats to Pre-Grant Opposition: Amendments to the Indian Patent Rules have made filing opposition to patents at the pre-grant stage more challenging.
- This change could lead to granting patents for inventions lacking genuine novelty or therapeutic efficacy.
- Impact on Competition and Drug Prices: Limitations to the pre-grant opposition process may stifle competition in the pharmaceutical market and contribute to higher drug prices.
- By hindering generic manufacturers and civil society organizations from challenging frivolous patents, the amendments impede the availability of affordable generic drugs.
- Pressure from Pharma Majors and International Trade Agreements: These amendments reflect pressure from multinational pharmaceutical corporations, particularly Western and Japanese companies, seeking to align India's patent rules with their interests.
- Their lobbying efforts aim to weaken India's patent regime, facilitating patent grants for incremental innovations and extending market exclusivity for their products.
- Threats to Flexibilities in Patent Law: Amendments to India's patent rules threaten the flexibilities inherent in its patent law, including provisions such as Section 3(d) that set stringent patentability criteria based on enhanced efficacy.
- Weakening these provisions undermines India's capacity to protect public health priorities and promote access to affordable medicines.
- Financial Burden on Opponents of Patents: Imposing fees on patent opponents could deter patients, civil society organizations, and generic manufacturers from filing pre-grant oppositions.
- This financial burden limits stakeholders' ability to safeguard public health interests and promote affordable medicines.
- Impact on Compulsory Licensing and Drug Availability: The amendments also affect the issuance of compulsory licenses, crucial for ensuring access to medicines when patents hinder availability.
- By weakening provisions that enable compulsory licensing and limit evergreening, the amendments impede efforts to address healthcare disparities and promote equitable access to essential medicines.
Conclusion
Access to affordable medicines is vital for public health and universal healthcare. Policymakers must preserve patent law flexibilities, promote competition, and protect patient interests to ensure healthcare systems uphold affordability, accessibility, and quality. Amendments to India's Patent Rules should balance innovation, intellectual property rights, and societal well-being, mitigating negative impacts on essential medicines and public health outcomes.
The Advent Of A Holistic Approach To 'One Health'

- 11 Apr 2024
Why is it in the News?
The ‘National One Health Mission’ is the result of the recognition that only a coordinated approach will ensure a better response to disease outbreaks.
Context:
- In recent times, the intricate relationship among humans, animals, and the environment has gained significant attention, especially in light of the emergence of pandemics like COVID-19.
- This interconnectedness is underscored by the impact of diseases such as lumpy skin disease, which affects both livestock productivity and trade, bridging the gap between domesticated and wild animal health.
- Addressing these complex challenges, the Indian government has launched the 'National One Health Mission,' aimed at comprehensively tackling the interlinked domains of human, animal, and environmental health.
What is One Health?
- One Health is an integrating idea that brings different sectors together to solve the health, productivity, and conservation challenges and has major implications for India.
- It is a global topic and was endorsed during India's presidency of the G-20.
- India with its diverse wildlife, one of the largest livestock populations, and high density of human population, carries heightened risks for inter-compartmental spread of diseases.
- The Covid pandemic, recent outbreaks of Lumpy Skin Disease in cattle, and the constant threat of Avian Influenza show that it is not just about addressing diseases from the human health point of view (zoonosis) but we need to address the livestock and wildlife aspects.
- This also opens opportunities for leveraging the complementarity and strengths that are inherent in each sector and devising integrated, robust, and agile response systems.
What is the National One Health Mission?
- Initiated in July 2022, the National One Health Mission represents a comprehensive endeavor endorsed by the Prime Minister's Science, Technology, and Innovation Advisory Council (PM-STIAC).
- With the participation of 13 ministries and departments, including the Department of Science and Technology, the Department of Biotechnology (DBT), and the Council of Scientific and Industrial Research (CSIR), among others, this mission adopts a holistic approach towards One Health and pandemic preparedness.
- A pivotal achievement within this mission is the establishment of the National Institute for One Health in Nagpur.
- Functioning as the central coordinating body for both national and international One Health endeavors, this institute marks a significant milestone in the mission's implementation.
- On December 11, 2022, the foundation stone of the institute was laid by the Prime Minister, symbolizing the commitment to advancing the principles of One Health and enhancing pandemic preparedness.
Objectives and Approaches of The National One Health Mission:
- Seamless Surveillance Integration: The mission endeavors to establish an integrated surveillance system that seamlessly monitors health indicators across human, animal, and environmental sectors.
- By amalgamating data from these domains, it can swiftly identify potential health hazards and respond proactively.
- Coordinated Outbreak Management: Recognizing the necessity of a unified approach in outbreak response, the mission aims to institute protocols and frameworks facilitating collaboration among various sectors.
- This coordinated effort enables effective resource and information sharing to mitigate the impact of diseases affecting multiple domains.
- Collaborative Research and Development: Through fostering collaboration among scientific research institutions and government bodies, the mission fosters the development of innovative solutions for emerging health threats.
- This includes the creation of vaccines, therapeutics, and diagnostics critical for pandemic preparedness and response.
- Seamless Information Exchange: Effective communication and data sharing are imperative for a unified One Health approach.
- The mission endeavors to facilitate seamless information exchange between sectors and stakeholders, ensuring timely and informed actions.
- Preparedness for Future Pandemics: Building on past pandemic experiences, the mission seeks to develop strategies and frameworks to enhance the country's readiness for future health crises.
- This involves proactive planning for potential pandemics and emerging diseases such as avian influenza or Nipah virus.
- Resource Optimization: By leveraging the resources and expertise of multiple sectors and stakeholders, the mission aims to optimize resource utilization, including laboratory infrastructure, healthcare facilities, and scientific research capabilities.
- This collaborative effort enhances efficiency and cost-effectiveness in addressing health threats.
- Public Health Education and Awareness: The mission includes public education initiatives to raise awareness about the interconnectedness of human, animal, and environmental health.
- Promoting an understanding of One Health principles encourages healthier behaviors and better preparedness for health emergencies.
Critical enabling activities of the One Health Mission:
- The outcomes of the One Health Mission will be supported by critical enabling initiatives.
- Many of these initiatives are ongoing and will be strengthened under the mission and several new activities that will facilitate the goals of the mission will be undertaken.?
Leveraging Laboratory Networks and Technological Integration in India's National One Health Mission:
- Establishment of High-Risk Pathogen Laboratories: The mission is dedicated to creating a nationwide network of laboratories equipped to handle high-risk pathogens classified under Biosafety Levels 3 and 4.
- These facilities provide a secure environment for studying infectious agents with pandemic potential.
- Departmental Collaboration: By consolidating laboratories managed by diverse departments, the mission aims to foster a cohesive network capable of coordinating resources and expertise across sectors.
- This integration enhances disease outbreak response, irrespective of its origin in human, animal, or environmental realms.
- Optimized Resource Allocation: Pooling laboratory resources within a unified network ensures efficient utilization of infrastructure and personnel.
- This collaborative approach enables swift responses to outbreaks and other health crises, maximizing available resources.
- Interdisciplinary Research and Analysis: Encouraging collaboration among experts from various disciplines—including medicine, veterinary science, environmental science, and public health—the mission promotes comprehensive research and analysis of health threats across multiple sectors.
- Integration of Artificial Intelligence (AI) and Machine Learning: Harnessing the power of AI and machine learning, the mission enhances epidemiological capabilities by analyzing vast datasets to detect patterns, trends, and potential health risks.
- This technology enables timely interventions and enhances overall preparedness.
- Utilization of Disease Modelling: Advanced modeling techniques are employed to forecast disease spread and potential outbreaks.
- These models facilitate targeted measures for disease control and prevention.
- Expansion of Genomic Surveillance: The mission broadens genomic surveillance efforts beyond COVID-19, encompassing other infectious diseases.
- By analyzing genetic material from diverse sources like wastewater and animal congregations, scientists can monitor disease prevalence and identify emerging threats.
- Capacity Building Initiatives: Emphasizing the importance of skill enhancement, the mission prioritizes capacity building across sectors in epidemiology, data analytics, and laboratory management.
- Training programs ensure that professionals possess the necessary skills to effectively utilize new technologies and methodologies.
Conclusion
The concept of One Health transcends mere disease management, encompassing broader realms such as antimicrobial resistance, food safety, plant diseases, and the consequential impacts of climate change. Addressing intersectoral issues like One Health necessitates active involvement not only from diverse governmental agencies but also from non-governmental organizations, academia, the private sector, and ordinary citizens. By adopting an actionable framework rooted in collaboration and comprehensive engagement, we can advance toward the overarching objectives of 'One Earth, One Health' and 'Health for All.
Shaping India’s path to inclusive health care

- 08 Apr 2024
Why is it in the News?
World Health Day, which is observed every year on April 7, unites us around health equity, an essential topic at the heart of global health and justice.
Context:
- World Health Day, commemorated every April 7th, underscores the significance of health equity, acknowledged as a basic human entitlement by the World Health Organization (WHO).
- Hence, it is imperative to delve into the theme "My Health, My Right," delving into the hurdles and remedies in attaining health equity in India.
- As a country contending with multifaceted socioeconomic inequalities in healthcare access and results, this exploration becomes pivotal.
What is Health Equity?
- Health equity, as outlined by the WHO, embodies the principle that every person should have the opportunity to attain optimal health, irrespective of their social, economic, or environmental circumstances.
- It extends beyond mere healthcare access, addressing underlying factors such as poverty, discrimination, and resource imbalances.
- Considering Diverse Health Outcomes: A core tenet of health equity acknowledges that health results stem from a multifaceted interplay of elements, encompassing social, economic, and environmental determinants.
- Individuals from disadvantaged backgrounds often encounter obstacles like financial constraints, transportation limitations, and sparse healthcare facilities.
- The Vitality of Health Equity: Health equity holds paramount importance not only ethically but also from a public health standpoint.
- Research consistently indicates that societies fostering greater health equity typically enjoy superior health outcomes, marked by lower morbidity and mortality rates, reduced healthcare expenditures, and heightened life expectancy.
- Conversely, persistent health disparities may precipitate societal unrest, economic strains, and a squandered human potential.
Health Equity Challenges in India:
- Addressing Urban-Rural Disparities: India contends with pronounced healthcare inequalities between urban and rural regions, where urban areas typically boast superior healthcare infrastructure and services, while rural communities encounter obstacles like limited access to facilities, healthcare professionals, and infrastructure, resulting in inferior health outcomes compared to their urban counterparts.
- Navigating Overcrowded Urban Slums: Urban slums present profound challenges characterized by extreme poverty, overcrowding, unsanitary conditions, and inadequate access to clean water, fostering the spread of infectious diseases and escalating morbidity and mortality rates.
- Moreover, deficient healthcare infrastructure exacerbates health disparities as residents grapple with limited access to essential services.
- Tackling Socioeconomic and Caste Disparities: Marginalized groups, including Scheduled Castes, Scheduled Tribes, and economically disadvantaged populations, confront elevated rates of illness and death due to restricted healthcare access, diminished health literacy, and societal prejudice.
- These disparities intertwine with broader determinants like education, employment, and housing, perpetuating disparities in health outcomes.
- Confronting the Burden of Non-Communicable Diseases (NCDs): Non-communicable diseases (NCDs) such as cardiovascular ailments, diabetes, and cancer pose a mounting challenge to health equity in India, constituting a substantial portion of the disease burden.
- However, marginalized communities often face barriers to accessing preventive measures and NCD treatment, amplifying health inequalities and exacerbating existing socioeconomic gaps.
- Navigating Shortages in Healthcare Personnel: A severe shortage of healthcare professionals, with only 0.8 doctors per 1,000 individuals according to WHO data, exacerbates health challenges, particularly in rural areas where access to primary care is limited, resulting in delayed diagnoses, substandard treatment, and compromised health outcomes.
- Confronting Infrastructure and Resource Limitations: Inadequate healthcare infrastructure, insufficient funding, and resource limitations pose formidable obstacles to health equity in India, with many public facilities lacking essential equipment, medications, and skilled personnel.
- Furthermore, the unequal distribution of resources aggravates urban-rural healthcare disparities, exacerbating inequities in access to quality healthcare services.
Strategies and Measures to Advance Health Equity in India:
- Enhancing Primary Healthcare Services: A pivotal approach to fostering health equity in India involves bolstering primary healthcare provisions, especially in rural and marginalized regions.
- This entails augmenting the accessibility and availability of primary care facilities, fortifying the skills and capabilities of frontline healthcare personnel, and ensuring the delivery of essential health services encompassing preventive care, maternal and child healthcare, and management of chronic ailments.
- Initiatives such as the National Rural Health Mission (NRHM) and the National Urban Health Mission (NUHM) strive to extend primary healthcare access and mitigate healthcare disparities between urban and rural locales.
- Advocating for Universal Health Coverage: Universal health coverage (UHC) stands as a cornerstone in ensuring equitable access to indispensable healthcare services devoid of financial strains.
- Endeavors like Ayushman Bharat, India's flagship health insurance program, aspire to furnish financial safeguarding to vulnerable segments by offering comprehensive coverage for hospitalization expenses.
- By broadening the reach of quality healthcare services and alleviating out-of-pocket costs, UHC endeavors to redress discrepancies in healthcare accessibility and enhance health outcomes for all citizens.
- Targeting Social Determinants of Health: Attaining health equity mandates a multifaceted approach that transcends healthcare interventions to address the underlying social determinants of health, encompassing poverty, education, housing, and employment.
- Initiatives geared towards poverty mitigation, augmenting educational and sanitation access, and fostering livelihood opportunities can wield a transformative impact on health outcomes and help ameliorate health disparities.
- Programs like the Mahatma Gandhi National Rural Employment Guarantee Act (MGNREGA) furnish rural households with employment prospects, thereby fostering enhanced socioeconomic circumstances and superior health outcomes.
- Empowering through Health Literacy: Elevating health literacy assumes paramount significance in empowering individuals to make informed health decisions and pursue equitable healthcare access.
- Integration of health education within prevailing healthcare schemes can heighten public consciousness and advocate for preventive healthcare practices.
- Fostering Collaborative Endeavors: Efficacious collaboration among governmental bodies, civil society, healthcare providers, and international entities constitutes a linchpin in addressing health inequities.
- By harnessing their respective competencies and resources, these stakeholders can conceptualize culturally sensitive health initiatives tailored to the distinctive requisites of diverse communities.
Conclusion
Realizing health equity in India necessitates coordinated endeavors spanning various sectors and involving diverse stakeholders. Through targeted interventions addressing socioeconomic health determinants, bolstering healthcare infrastructure, and fostering collaborative alliances, India can progress towards a future where equitable access to superior healthcare becomes a universal norm. The pursuit of health equity transcends moral imperatives, emerging as a pivotal prerequisite for fostering sustainable development and societal advancement.
How the Government Can Generate Employment Through Universal Healthcare

- 05 Apr 2024
Why is it in the News?
As India approaches the 2024 elections, highlighting healthcare as a strategic investment rather than a fiscal burden can drive employment generation, bolster economic growth, and foster sustainable development.
Context:
- With India gearing up for the upcoming general elections, recognizing healthcare as a crucial investment for national well-being and prosperity is essential.
- Despite its pivotal role, healthcare tends to be sidelined in political discussions, necessitating a shift in focus.
- Rather than perceiving healthcare as a financial burden, it should be considered a strategic investment.
- Embracing healthcare as an investment offers substantial returns, contributing to human capital development, economic progress, and sustainable development.
What is Universal Health Care (UHC)?
- Universal Health Care (UHC) embodies the principle that everyone should have access to quality healthcare regardless of financial situation.
- It is regarded as a fundamental measure for promoting human equity, security, and dignity.
- UHC has gained widespread acceptance as a primary goal of public policy globally, with numerous countries successfully implementing it, including wealthier nations and emerging economies like Brazil, China, Sri Lanka, and Thailand.
- World Health Organization (WHO) defines universal healthcare as “all people and communities can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship.”
Challenges in Implementing Universal Health Care (UHC):
- Inequitable Access to Health Insurance: Disparities in health insurance coverage persist, with the lowest wealth quintile and marginalized sections facing limited access to insurance, as indicated by NFHS-5 results.
- Lack of Financial Protection: Despite initiatives like Janani Shishu Suraksha Karyakram, high out-of-pocket expenses, especially in urban areas, pose financial risks. NFHS data highlights significant disparities in expenditure across states.
- Inclusion and Exclusion Errors in Health Insurance Policies: Inaccuracies in health insurance policies, including PMJAY, lead to the inclusion of ineligible and exclusion of eligible households, affecting coverage effectiveness.
- Availability of Services: While PMJAY enlists hospitals, a significant portion is in the private for-profit sector, potentially limiting access to underserved areas.
- Inadequate Infrastructure: Insufficient healthcare facilities, equipment, and medical supplies hinder UHC implementation, compounded by a shortage of specialists in CHCs.
- Poor Health Education: Limited awareness about preventive health measures contributes to preventable illnesses, emphasizing the need for improved health education and promotion.
Steps For Achieving Universal Health Care (UHC):
- Increase in Public Health Expenditure: Commitment to allocate 2.5% of GDP to health by 2025 is crucial.
- However, the current central budget allocation for 2024-25 falls short at 28%.
- Strategic Partnerships: The government must forge partnerships and incentivize the private sector to bridge healthcare gaps.
- Initiatives like Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) illustrate this collaborative approach, covering over 60 crore people.
- Reimbursement Rates Correction: Private sector participation is hindered by low reimbursement rates.
- Differential pricing based on clinical excellence and infrastructure investment can encourage participation.
- Infrastructure Development: Addressing the deficit of nearly 24 lakh hospital beds requires increased private sector investment, especially in tier 2 and 3 cities.
- National Priority Status for Healthcare: Designating healthcare as a national priority sector can unlock funding opportunities and incentives, fostering growth and development.
- Strengthening Primary Healthcare: Enhancing Health and Wellness Centers and including OPD care in health insurance coverage will improve health outcomes and reduce secondary and tertiary care burdens.
- Prevention and Control of NCDs: Prioritizing interventions at the primary healthcare level can significantly reduce the burden of non-communicable diseases, preventing complications and hospitalizations.
- Boosting Private Investment: Encourage and incentivize private sector investment in healthcare infrastructure, technology, and services to expand coverage and enhance healthcare accessibility and affordability for all citizens.
How Government can Generate Employment Through UHC in India?
Expanding the Healthcare Workforce: Universal healthcare will significantly increase the demand for healthcare professionals, creating millions of new jobs. This includes doctors, nurses, paramedics, technicians, pharmacists, and other support staff. The government can address this need by:
- Scaling Up Medical Education: Increased investment in medical colleges and nursing schools is crucial.
- This includes establishing new institutions, expanding existing ones, and introducing scholarship programs to attract talent.
- Standards for medical education must be maintained to ensure a high-quality workforce.
- Skill Development Initiatives: Developing a robust skill development ecosystem specific to healthcare is essential.
- This involves creating standardized training programs for various healthcare professions.
- Skill development should not be limited to clinical skills but also encompass areas like communication, empathy, and public health awareness.
- Attracting and Retaining Talent: Competitive salaries, loan repayment programs, and career progression opportunities can incentivize students to pursue healthcare careers.
- Additionally, considering the rural-urban divide, special incentives like higher pay and improved living conditions can attract healthcare professionals to serve in underserved areas.
Building a Robust Healthcare Infrastructure: Universal healthcare necessitates a well-developed healthcare infrastructure. This translates to significant job creation across various sectors:
- Infrastructure Development: Building new hospitals, clinics, diagnostic centers, and public health centers requires construction workers, engineers, architects, and technicians.
- Medical Equipment Manufacturing: Increased demand for medical equipment, from basic diagnostic tools to advanced technology, can incentivize local manufacturing.
- This can create numerous jobs in production, maintenance, and research & development.
- Pharmaceutical Industry: Universal healthcare will significantly raise the demand for pharmaceuticals.
- This can boost domestic production, generating jobs in manufacturing, distribution, and research & development.
The Role of Public-Private Partnerships (PPPs):
- The government cannot shoulder the entire responsibility alone. PPPs can play a vital role in expanding healthcare infrastructure and creating job opportunities:
- Strategic Partnerships: Collaboration with private hospitals and clinics can leverage existing infrastructure and expertise.
- The government can purchase services from the private sector, ensuring wider reach and quality care, while creating jobs within these institutions.
- Incentivizing Expansion: Tax breaks, subsidies, and streamlined licensing processes can incentivize private players to expand their facilities and hire more staff.
- This creates a multiplier effect, leading to job creation in construction, logistics, and other associated sectors.
Technology and its Role in Employment: Technology holds immense potential to improve healthcare delivery and create new job opportunities:
- Telehealth and Digital Health Records: Investment in telemedicine infrastructure and digital health records can create jobs in IT, data management, and cybersecurity.
- Additionally, telemedicine can bridge the gap in rural healthcare, requiring trained personnel to operate these services.
- Medical Informatics: The use of big data and analytics in healthcare will require skilled professionals to collect, analyze, and interpret data to improve healthcare delivery and outcomes.
Conclusion
Universal healthcare in India can be a transformative force, not just for public health, but also for the nation's economic landscape. By strategically investing in workforce development, fostering public-private partnerships, and embracing technological advancements, India can unlock a vast employment potential. This not only creates a win-win for job creation and healthcare access but also paves the way for a healthier and more prosperous future for all Indians.
India’s HIV/AIDS Response
- 01 Apr 2024
Why is it in the News?
April 1, 2004, marked a significant moment in India's fight against HIV/AIDS as Free Antiretroviral Therapy (ART) was introduced for Persons Living with HIV (PLHIV).
Context:
- April 1, 2004, stands as a landmark moment in India's approach to addressing the HIV/AIDS epidemic, as Free Antiretroviral Therapy (ART) was introduced for Persons Living with HIV (PLHIV).
- This initiative, conceived in response to the pressing issues of access and affordability, has emerged as a crucial intervention in the fight against the disease.
- As we commemorate this day, it is imperative to delve into the progression and significance of India's free ART program, shedding light on its transformative impact on the nation's response to the HIV/AIDS crisis.
HIV/AIDS's Emergence and Initial Challenges:
- Inception of a Global Health Crisis: The emergence of HIV/AIDS in the early 1980s signaled the onset of a widespread health emergency with profound implications for populations worldwide.
- Originally detected among groups in the United States, the disease swiftly traversed borders, reaching nations like India and beyond.
- This era was characterized by uncertainty, anxiety, and a lack of comprehension regarding the novel virus, initially dubbed GRID (Gay-Related Immune Deficiency), later renamed HIV (Human Immunodeficiency Virus) and its associated illness AIDS (Acquired Immunodeficiency Syndrome).
- Absence of Effective Treatments Resulting in Dire Consequences: During the initial stages of the epidemic, HIV/AIDS was synonymous with a dire prognosis, largely due to the absence of viable treatment options.
- Marginalized communities, including men who have sex with men, intravenous drug users, and commercial sex workers, bore the brunt of the disease's impact.
- However, as time progressed, it became evident that HIV/AIDS transcended boundaries of gender, sexual orientation, and socioeconomic status, affecting individuals from diverse backgrounds.
- Pervasive Social Stigma: In addition to its grave health implications, HIV/AIDS precipitated significant social stigma and discrimination.
- Individuals living with HIV/AIDS encountered marginalization, employment loss, and social exclusion from both their communities and families.
- This pervasive stigma compounded the challenges associated with managing HIV/AIDS and impeded effective epidemic control efforts.
- Limited Treatment Accessibility and Exorbitant Costs of Available ART: Despite the escalating recognition of HIV/AIDS as a global health threat, access to treatment remained scant, particularly in low- and middle-income nations such as India.
- The approval of the first antiretroviral drug, AZT (zidovudine), by the US Food and Drug Administration (US FDA) in March 1987 marked a significant milestone.
- HAART (Highly Active Antiretroviral Therapy) represented a breakthrough in disease management, combining multiple antiretroviral drugs to suppress viral replication and bolster immune response.
- However, the exorbitant expenses associated with HAART, reaching up to $10,000 annually per patient, rendered it inaccessible to the majority of individuals living with HIV/AIDS, especially those residing in resource-constrained settings.
The Introduction of Free ART in India and its Impact:
- In response to the pressing issues of limited access and affordability of HIV/AIDS treatment, the Indian government embarked on a significant initiative.
- On April 1, 2004, the government initiated the provision of Free Antiretroviral Therapy (ART) for Persons Living with HIV (PLHIV).
- The introduction of Free ART aimed to dismantle barriers to treatment and extend life-saving medication to all PLHIV, irrespective of their financial means.
- By offering ART at no cost, the government endeavored to ensure that access to treatment would not be hindered by financial constraints, thereby addressing a crucial gap in healthcare accessibility.
Its Role in Curbing the Epidemic
- Enhanced Treatment Accessibility: Over the past two decades, the initiative has undergone substantial expansion, witnessing a surge in the number of ART centers from less than 10 to approximately 700, catering to around 1.8 million PLHIV.
- This proliferation has facilitated heightened treatment access for individuals living with HIV/AIDS nationwide, including those residing in remote and underserved regions.
- A notable outcome of the Free ART endeavor has been the remarkable enhancement in health outcomes observed among PLHIV.
- Significant Reduction in Mortality Risk and Transmission Rates: Timely and effective treatment accessibility has transfigured HIV/AIDS from a dire prognosis to a manageable chronic ailment for many.
- By suppressing viral load and bolstering immune response, ART has not only extended the lifespan of PLHIV but also augmented their quality of life.
- Moreover, the Free ART initiative has played a pivotal role in curbing HIV transmission rates by ensuring treatment access for PLHIV, thereby thwarting virus dissemination within communities.
- Research indicates that efficacious ART can substantially mitigate HIV transmission risk, contributing to the overall decline in HIV prevalence.
- Broader Societal Benefits: Beyond its direct impact on individuals grappling with HIV/AIDS, the Free ART initiative has yielded wider societal advantages.
- By mitigating the disease burden and forestalling fresh infections, the initiative has alleviated the societal and economic repercussions of HIV/AIDS on families, communities, and healthcare systems.
- Supplementary Measures and Patient-Centric Approach: The success of India's ART program extends beyond free medication provision.
- Complementary initiatives, such as complimentary diagnostic services, prevention of parent-to-child transmission programs, and management of opportunistic infections, have played pivotal roles in curbing the HIV epidemic.
- Furthermore, the program has adopted a patient-centric strategy, furnishing stable PLHIV with two to three months' worth of medicines to minimize clinic visits and enhance treatment adherence.
Challenges and Future Prospects:
- Delayed Initiation and Attrition in Care: A notable portion of patients presents with advanced HIV illness, evidenced by low CD4 counts, impacting treatment efficacy.
- Furthermore, attrition in care remains a concern, as some patients discontinue treatment upon feeling well, leading to interruptions and potential drug resistance development.
- Logistical Hurdles and Infrastructure Deficiencies: Remote and underserved regions, including those with rugged terrain, encounter hurdles in accessing vital medications and healthcare provisions.
- Fortifying the logistical network and infrastructure for dispensing ART drugs is imperative to sustain uninterrupted treatment access for all PLHIV.
- Involvement of the Private Sector: While the public sector assumes a pivotal role in HIV/AIDS treatment provision, fostering collaboration with the private sector is crucial.
- Leveraging the resources and infrastructure of private healthcare entities can expand ART accessibility and reach marginalized populations, including urban dwellers.
- Interconnected Health Program Integration: Augmenting integration with other health initiatives, encompassing hepatitis, non-communicable ailments, and mental health, holds paramount importance.
- Given PLHIV's propensity for concurrent ailments, comprehensive and integrated healthcare services necessitate intersectoral collaboration within the healthcare spectrum.
- Realization of Ambitious NACP Phase 5 Objectives: The ongoing fifth phase of the National AIDS Control Programme (NACP) sets forth ambitious targets, envisaging an 80% reduction in annual new HIV infections and AIDS-related mortalities by 2025.
- Achieving these milestones demands concerted endeavors to escalate testing, enhance treatment coverage, and secure viral suppression among PLHIV.
Conclusion
India's free ART initiative has successfully combated HIV/AIDS, demonstrating the power of accessible healthcare. Its achievements emphasize the importance of political will, funding, community engagement, and patient-centered care in tackling infectious diseases. Lessons from this program will guide future public health endeavors, improving outcomes for all
TB-Mukt Bharat India's Fight Against Tuberculosis
- 26 Mar 2024
Why is it in the News?
Even though World TB Day (March 24) has passed, recognizing the needs and interests of patients and communities must form the basis of disease elimination.
What is Tuberculosis?
- Tuberculosis (TB) is an airborne bacterial infection caused by a type of bacteria called mycobacterium tuberculosis.
- The infection primarily attacks our lungs and if not treated early, permanent lung damage can result.
- Tuberculosis can also spread to other parts of the body such as the intestines, bones and joints, brain, skin, and other tissues of the body.
- It can be classified into two categories:
- Active tuberculosis (TB) and
- Latent tuberculosis (TB).
Causes of Tuberculosis (TB):
- Mycobacterium tuberculosis usually spreads from person to person through airborne droplets, which are produced when the infected person coughs, sneezes, speaks, or sings.
Signs & symptoms of Tuberculosis (TB):
- A person with latent Tuberculosis (TB) cannot spread the infection to others as it is not contagious and may not show symptoms because their immune system is protecting them from getting sick.
- However, latent TB can develop into active TB if that individual’s immune system cannot stop the bacteria from growing and starts showing symptoms such as:
- Bad cough that lasts for 3 weeks or longer
- Pain in chest
- Coughing blood or sputum
- Fever or night sweats
- Weight loss or no appetite
- Chills
- Weakness
Diagnosis of Tuberculosis (TB):
- Tuberculosis (TB) can be tested in two ways, namely skin test and blood test.
- These two tests only tell if a person has TB or not; if the test is positive then other tests are needed to check if it is latent TB or active TB, such as chest X-ray or CT, or acid-fast bacillus tests (sputum tests).
Treatment of Tuberculosis (TB)
- Both latent TB and active TB can be effectively treated with antibiotics, albeit requiring different durations of treatment.
- Complete adherence to medication is imperative for curing TB; failure to complete the prescribed course may lead to the recurrence of illness and increased difficulty in recovery.
- For latent TB, treatment typically involves a course lasting 3-9 months, comprising 1-2 antibiotics.
- While active TB necessitates a more extensive regimen, with doctors prescribing 2 to 4 or more antibiotics for 6-9 months or longer.
- Ensuring proper medication adherence is crucial for individuals with latent TB to prevent its progression to active TB.
- In many cases, significant improvement is observed within weeks of initiating treatment, with the infection becoming non-contagious.
- Therefore, completing the full course of medication is essential to safeguard oneself and others from tuberculosis.
What is drug-resistant Tuberculosis (TB)?
- Drug-resistant TB is when the bacteria that causes TB becomes resistant to some or all the medications.
- Once drug-resistant TB is developed, it is very difficult to treat it.
- It may require more and different medications with a longer period of treatment.
- Some injectable drugs can cause loss of hearing and balance problems.
Status of TB in India:
- India bears approximately 27% of the global burden of tuberculosis (TB), making it the country with the highest TB burden worldwide.
- Government of India aims to eliminate tuberculosis (TB) by 2025.
- The theme for World Tuberculosis Day (March 24) in 2024 was the same as in 2023 “Yes, we can end TB”, which reflects the United Nations Sustainable Development Goals (SDGs) to eliminate TB by 2030.
Challenges Confronting India in TB Elimination:
- Drug-resistant TB Cases: India grapples with a substantial burden of drug-resistant TB, including multidrug-resistant TB (MDR-TB), necessitating more expensive, specialized drugs and prolonged treatment durations.
- Diagnostics and Case Detection: Accurate and timely TB diagnosis remains a challenge, particularly in areas lacking access to modern diagnostic tools, leading to reliance on older, less reliable methods.
- Poor Primary Healthcare and Infrastructure: Limited access to healthcare facilities, especially in rural and remote regions, results in delayed diagnosis and treatment, facilitating TB transmission within communities.
- Stigma and Awareness: Stigma surrounding TB may deter individuals from seeking timely healthcare, while inadequate awareness about the disease perpetuates its prevalence.
- Private Sector Engagement: With a significant portion of healthcare services provided by the private sector, effective TB control necessitates coordinated efforts and standardized treatment protocols between the public and private sectors.
- Treatment Adherence: Ensuring patient adherence to the full course of TB treatment, which involves prolonged antibiotic courses, poses a significant challenge.
- Vulnerable Populations: Certain demographics, such as migrant workers, urban slum dwellers, and individuals residing in overcrowded conditions, face heightened TB risks, requiring targeted interventions.
Initiatives by the Government of India to Eradicate TB:
- National Tuberculosis Elimination Program (NTEP): A National Strategic Plan (2017-25) aims to eliminate TB from India by 2025.
- Pradhan Mantri TB Mukt Bharat Abhiyan (PMTBMBA): Introduced in 2022, this initiative provides community support to TB patients, offering nutritional, diagnostic, and vocational assistance.
- Revised National Tuberculosis Control Program (RNTCP): Launched in 1997, RNTCP has been continuously revised and strengthened to combat TB effectively.
- Universal Drug Susceptibility Testing (DST): Efforts have been intensified to ensure universal access to drug susceptibility testing, enabling early detection of drug-resistant TB strains for tailored treatment.
- Ni-kshay Portal: An online platform established to monitor notified TB cases effectively.
- Introduction of New Drugs: Drugs like Bedaquiline and Delamanid for treating drug-resistant TB are provided free of cost to TB patients.
- Research and Development (R&D) for Treatment: Studies are ongoing to explore shorter anti-tubercular drug courses, aiming to reduce treatment duration.
- Vaccine Development: Trials are being conducted to evaluate the effectiveness of vaccines such as Immuvac and VPM1002 in preventing TB, offering promising avenues for future TB prevention strategies.
Global Efforts to Eradicate TB:
- End TB Strategy: spearheaded by the World Health Organization (WHO), it provides a roadmap for countries to reduce TB incidence by 80%, and TB deaths by 90%, and eliminate catastrophic costs for TB-affected households by 2030.
- World Development Report (1993): Published by WHO, it highlighted TB treatment for adults as the most cost-effective among all developmental interventions.
- The Global Fund: a global initiative aimed at defeating HIV, TB, and malaria, striving for a healthier, safer, and more equitable future worldwide.
- The Stop TB Partnership: a collaborative effort involving expertise from diverse country, regional, and global partners, dedicated to transforming the TB landscape and achieving the goal of ending TB by 2030.
- Sustainable Development Goal 3: part of the United Nations' Sustainable Development Goals, it targets to end the TB epidemic by 2030, reflecting a commitment to global health and well-being.
Way Forward:
- Development and Widespread Adoption of an Adult TB Vaccine: Prioritizing the research and development of an effective vaccine against TB for adults.
- Ensuring widespread distribution and utilization of the vaccine to bolster TB prevention efforts globally.
- Cost Reduction of Anti-TB Drugs: Implementing strategies to lower the production costs of essential anti-TB medications.
- Making these drugs more accessible and affordable to all individuals in need, regardless of economic status.
- Innovation in TB Treatment: Investing in research and development to create injection-free and orally-administered TB medications.
- Expanding treatment options to enhance patient compliance and improve treatment outcomes.
- Integration of AI-Assisted Radiology: Leveraging artificial intelligence (AI) technology to facilitate rapid and accurate TB diagnosis.
- Promoting the use of handheld radiology devices equipped with AI algorithms, allowing for quick TB detection with high accuracy rates, thereby streamlining diagnostic processes and improving patient care.
Populism and Health Inequality in India (The Hindu)

- 30 Jan 2024
Why is it in the News?
A fair and effective health system requires freedom from political influence, focusing on policymaking and implementation driven by scientific evidence and long-term objectives.
Background:
- Within India's diverse landscape, where bustling cities coexist with serene villages, there's a subtle yet crucial struggle unfolding in the realm of public health.
- Despite its significance, this battle often takes a backseat to the allure of curing illnesses. While disease prevention holds paramount importance, political attention tends to gravitate towards visible and immediate achievements such as constructing new medical facilities, offering affordable treatments, and managing crises.
- Hence, there arises a pressing need to examine the challenges and deficiencies within the existing democratic approach to public health, emphasizing the necessity for evidence-based strategies geared towards long-term objectives.
What is the Present Condition of Public Health and Nutrition in India?
- According to the 5th National Family Health Survey 2019-21:
- 35.5% of children under 5 exhibited stunted growth.
- 32.1% were underweight.
- The prevalence of anaemia among children aged 6-59 months rose from 58.6% to 67.1%.
- Among women aged 15-19 years, the prevalence of anaemia increased from 54.1% to 59.1%.
- These statistics underscore a notable disparity in public health endeavours.
The Incongruity of the Democratic Process in India's Public Health:
- Emphasis on Infrastructure and Immediate Relief: The inclination towards constructing new hospitals and providing subsidized treatments reflects democratic governance in India.
- While these initiatives address immediate healthcare needs, their impact on sustained population health still needs to be improved.
- During health crises, political leaders often prioritize emergency response strategies, swiftly mobilizing state resources.
- However, many of these measures yield minimal impact due to insufficient follow-through beyond public announcements.
- Preferring Emergency Response over Vital Preventive Measures: Budget constraints often limit the effective implementation of announced initiatives, raising concerns about their long-term sustainability and impact.
- This emphasis on visible achievements can overshadow critical areas like sanitation, disease surveillance, and public health education.
- Yet, these aspects are vital for maintaining population health and averting disease outbreaks.
- The significance of quieter victories achieved through preventive measures, such as eradicating diseases like smallpox and controlling polio, often goes unnoticed despite their substantial contributions to public well-being.
A Case Study of Dengue Illustrating This Dilemma
- Immediate Response Emphasis: During dengue outbreaks, political leaders often prioritize swift relief actions, such as establishing relief camps and offering symptomatic treatments.
- This reactive stance arises from the urgency of the situation and the imperative to alleviate the immediate suffering of affected communities.
- However, the lack of emphasis on preventive measures can perpetuate a cycle of recurrent outbreaks, straining healthcare resources further.
- Overlooking Underlying Causes and Prevention: The focus on emergency relief efforts may overshadow the significance of long-term strategies, including studying vector bionomics, developing vaccines, and enhancing public health infrastructure.
- Consequently, the current approach falls short of averting future outbreaks and burdens the healthcare system.
- Research and development in these realms are imperative. For instance, despite limitations, the existing dengue vaccine underscores the necessity for further exploration.
- Additionally, climate change impacts mosquito breeding and movement patterns, necessitating adaptations in public health strategies.
What are the challenges in Public Health in India:
- Prioritizing Short-Term Gains: Political leaders often prioritize initiatives promising immediate results, like constructing new hospitals and offering subsidized treatments, over long-term public health strategies.
- Budgetary Limitations: Despite announcements, the impact of these short-term measures is limited due to constraints in budget allocation and implementation beyond public announcements.
- Neglect of Vital Areas: Critical aspects such as sanitation, disease surveillance, and public health education are often overlooked, despite their significance in maintaining population health and preventing disease outbreaks.
- For example, in the case of Dengue, relief efforts overshadow long-term strategies like vector control and vaccine development.
- Profit-Driven Pharmaceutical Sector: The profit-oriented nature of the pharmaceutical industry sidelines public health priorities, leading to disparities in medicine availability, particularly concerning diseases like tuberculosis, which disproportionately affect socio-economically disadvantaged populations.
- Lack of Holistic Approach: Addressing public health challenges necessitates interdisciplinary expertise from fields like environmental science, sociology, urban planning, and economics.
- However, India's current approach remains predominantly physician-centric, overlooking broader societal and environmental factors.
What Steps Can Be Taken?
- Prioritize Research and Development: Emphasize research, particularly in vaccine development and understanding the influence of climate change on disease vectors, to inform proactive public health strategies.
- Depoliticize Health Decision-Making: Ensure that public health policies are driven by scientific evidence and long-term objectives rather than short-term political considerations.
- Enhance Nutrition Support: Increase investments in nutrition programs, recognising their significant long-term benefits for health and productivity.
- Adopt a Holistic Approach: Implement a comprehensive public health management strategy that encompasses preventive measures, policy development, community health initiatives, and environmental health considerations.
- Grant Autonomy to Health Ministries: Consider granting health ministries greater autonomy, potentially placing them directly under the leadership of elected officials such as Chief Ministers or Prime Ministers, similar to India’s space and atomic energy departments, to facilitate more effective decision-making and implementation processes.
Conclusion
Although democracy itself is not detrimental to public health, the existing approach within democratic frameworks frequently lacks effectiveness. There is a pressing requirement to rethink public health governance, prioritizing evidence-based, comprehensive, and forward-looking strategies that cater to both present and future health requirements.
What are the Pollutants in Our Air, and How They Impact Health (Indian Express)
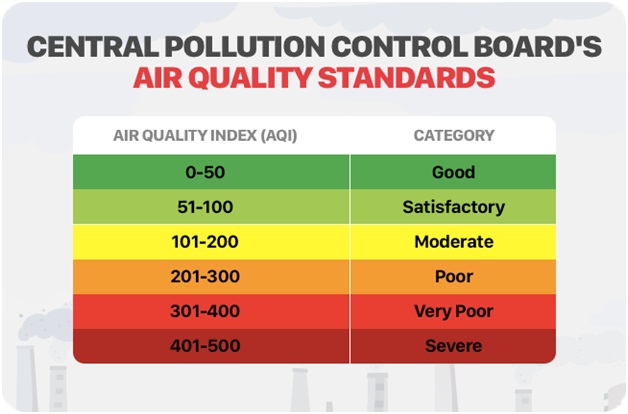
- 08 Nov 2023
Why is it in the News?
Rising pollution levels in north India have led to focus returning on the Air Quality Index (AQI) score, a measure of air pollution.
Context:
- The escalating pollution in northern India has once again drawn attention to the Air Quality Index (AQI) score, which gauges air pollution levels.
- On Monday, Delhi, for instance, registered an AQI score exceeding 400.
- This categorizes the air quality as 'severe,' with any reading above 100 indicating at least a moderate level of pollution on the index.
What is the Air Quality Index (AQI)?
- AQI is a number, which is a measure of air quality.
- The higher the AQI, the worse the air.
- The color-coded AQI index was launched in India in 2014, and it helps the public and the government understand the condition of the air and what subsequent measures are to be taken to combat the situation, based on its severity.
- According to the Central Pollution Control Board, part of the Ministry of Environment, Forests, and Climate Change, the AQI transforms complex air quality data of various pollutants into a single number (index value), nomenclature, and color.
- The pollutants measured include PM 10, PM 2.5, Nitrogen Dioxide, Ozone, Carbon, etc.
- There are six categories of AQI, namely ‘Good’ (0-50), ‘Satisfactory’ (51-100), ‘Moderately polluted’ (101-200), ‘Poor’ (201-300), ‘Very Poor’ (301-400), and ‘Severe’ (401-500).
How Pollutants Impact Our Health?
PM 10 and PM 2.5
- These are extremely fine particulate matter (PM) particles, with the digits accompanying them referring to their diameter.
- So, PM 10 and PM 2.5 are smaller than 10 and 2.5 microns in their diameter, respectively.
- One micron is about a thousandth of a millimeter and this tiny size has a role to play in how they impact human health.
- The finer the particles are, the more difficult it gets to protect oneself from them.
- Due to their size, the PM 2.5 particles can easily bypass the nose and throat and can enter the circulatory system.
- The particles can also lead to chronic diseases such as asthma, heart attack, bronchitis, and other respiratory problems.
- Byproducts of emissions from factories, vehicular pollution, construction activities, and road dust, such particles are not dispersed and stay suspended in the air that we breathe.
Nitrogen Dioxide (NO2)
- Nitrogen dioxide (NO2) gets in the air from the burning of fuel, with sources including emissions from vehicles and power plants.
- Short-term exposure to high levels of NO2 can aggravate respiratory diseases like asthma, and lead to other problems such as coughing or difficulty in breathing.
- Long-term exposure may also contribute to the development of asthma and could increase susceptibility to respiratory infections.
Ozone (O3)
- Ozone is a gas that is present in the upper layers of the atmosphere, protecting human health from the impact of the Sun’s UV rays.
- However, surface-level ozone is among the most significant air pollutants. It is formed by the reaction of atmospheric pollutants in the presence of sunlight.
- According to the International Journal of Medical Public Health, with the increase in surface ozone levels, there is a likelihood of an increase in the risk of hospital admissions for Chronic Obstructive Pulmonary Diseases (COPD) and the number of cardiovascular and respiratory deaths.
Sulphur Dioxide (SO2)
- The largest source of SO2 in the atmosphere is the burning of fossil fuels by power plants and other industrial facilities.
- Additional sources are industrial processes and natural sources such as volcanoes.
- As with other gases, SO2 exposure is harmful to the cardiovascular system and can lead to the development of respiratory illnesses.
- SO2 can also react with other compounds to form particulate matter.
- At high concentrations, gaseous SOx can harm trees and plants by damaging foliage and decreasing growth.
Ammonia (NH3)
- A 2017 NASA-funded study said that in India, “A broad increase in fertilizer use coupled with large contributions from livestock waste have resulted in the world’s highest concentrations of atmospheric ammonia.”
- While gaseous ammonia is a natural part of Earth’s nitrogen cycle, excess ammonia is harmful to plants and reduces air and water quality.
- In the troposphere –where all weather takes place and where people live – ammonia gas reacts with nitric and sulfuric acids to form nitrate-containing particles.
- Those particles contribute to aerosol pollution that is damaging to human health.
- Ammonia gas can also fall back to Earth and enter lakes, streams, and oceans, where it contributes to harmful algal blooms and “dead zones” with dangerously low oxygen levels.
Lead (Pb)
- Lead is a naturally occurring toxic metal found in the Earth’s crust. But in increased quantities, exposure to it becomes extremely dangerous to health.
- Important sources of environmental contamination come from mining, smelting, manufacturing and even recycling activities.
- Young children are particularly vulnerable to lead poisoning because they absorb four to five times as much ingested lead as adults from a given source.
- Children who survive severe lead poisoning may be left with permanent intellectual disability and behavioral disorders.
Carbon Monoxide (CO)
- A toxic, colorless, and odorless gas, it is given off when fuel containing carbon, such as wood, coal, and petrol, is burned.
- If CO levels are high enough, a person may become unconscious and die. Long-term exposure has been linked with an increased risk of heart disease.
Delhi Air Pollution: Causes, Impact & Measures (The Hindu)

- 04 Nov 2023
Why is it in the News?
The air quality in Delhi-NCR declined over the past week due to a gradual drop in temperatures, calm winds that trap pollution, and a surge in post-harvest paddy straw burning across Punjab and Haryana.
Context:
- The air quality in Delhi has plummeted to hit the ‘severe’ category for the first time this season, with the AQI breaching the 450 mark according to the Central Pollution Control Board (CPCB).
- The State government implemented restrictions, including banning construction and demolition activities.
- Over the last few years, Delhi and its surrounding areas have been subject to hazardous smog, which conincides with the winter months rolling in.
- Smoke from farmers burning crop stubble, vehicle exhaust and factory emissions combine every winter to blanket the region in a toxic haze.
What is Pollution?
- Pollution refers to the contamination of the earth's environment with materials that interfere with human health, quality of life or the natural functioning of the ecosystems.
- The major forms of pollution include water pollution, air pollution, noise pollution and soil contamination.
- Other less-recognised forms include thermal pollution and radioactive hazards.
What are the Reasons behind Rising Air Pollution in Delhi?
- Delhi is one of the most polluted capital cities in the world for a variety of factors, including location (landlocked city), traffic patterns, dust, and farm fires.
- However, weather also has a significant impact.
- Typically, Delhi experiences deteriorating air quality from October to November, with improvements occurring from March to April.
- Unlike the winter season, the current weather conditions are not unfavorable.
- During winter, cool and calm weather tends to trap and intensify daily pollution, especially in northern India within the Indo-Gangetic Plain.
- In addition to local emissions, the decline in air quality is primarily attributed to an increase in fire incidents, largely resulting from the burning of wheat crop stubble in northern India especially Punjab and Haryana.
- Air Pollution in Delhi-NCR and the Indo-Gangetic Plains is a complex issue influenced by a variety of factors.
- Location: Delhi is a landlocked city compared to Mumbai and Kolkata so the level of pollution is more as the level of particulate matter and pollutants is not able to get discharged into the surrounding areas.
- Wind Direction: In October, the monsoons withdraw from Northwest India, bringing northwesterly winds.
- During summers, northwesterly winds transport dust from northern Pakistan and Afghanistan.
- Reduced Wind Speed: Winters see lower wind speeds compared to summers, making the region more susceptible to pollution.
- Delhi's landlocked position doesn't benefit from the sea breeze that disperses pollutants in other parts of the country.
- Stubble Burning: Burning crop stubble in states like Punjab, Rajasthan, and Haryana adds to the winter smog.
- This practice releases harmful gases like methane, carbon monoxide, volatile organic compounds, and carcinogenic polycyclic aromatic hydrocarbons.
- Vehicular Pollution: Vehicular emissions significantly contribute to declining air quality in Delhi during winter, accounting for about 20% of the problem.
- Dust Storms: Dust storms from Gulf countries worsen the existing pollution levels.
- Dry and cold weather results in dusty conditions from October to June, contributing to PM10 and PM2.5 pollutants.
- Temperature Drop: Lower temperatures reduce the inversion height, concentrating pollutants in the lower atmosphere.
- The inversion height is the layer beyond which pollutants cannot disperse upward.
- Firecrackers: Despite bans on firecracker sales, Diwali celebrations with fireworks contribute to air pollution.
- Construction Activities and Open Waste Burning: Large-scale construction projects in Delhi-NCR increase dust and pollution.
- Landfill sites and open waste burning also add to air pollution concerns.
Impact of Air Pollution on health:
- Respiratory Issues: Air pollution is a major cause of respiratory problems, including asthma, bronchitis, and lung infections.
- It can exacerbate existing conditions and increase the risk of developing them.
- Cardiovascular Diseases: Poor air quality is linked to heart problems, including heart attacks and stroke, as it can lead to the buildup of plaque in blood vessels and raise blood pressure.
- Cancer Risk: Long-term exposure to certain air pollutants is associated with an increased risk of lung and other types of cancer.
- Neurological Effects: Emerging research suggests that air pollution may have adverse effects on the central nervous system and could be linked to cognitive decline and mental health issues.
- Reduced Life Expectancy: Prolonged exposure to air pollution is associated with a shortened life expectancy, as it contributes to a range of health problems that can be life-threatening.
Impact of Air Pollution on Economic Growth:
- Healthcare Costs: Air pollution increases medical expenses due to illnesses, reducing economic growth.
- Lower Productivity: Poor air quality impairs worker productivity, hampering economic output.
- Tourism and Investment: Severe pollution deters tourists and investors, affecting local economies.
- Agricultural Losses: Air pollution harms crops, impacting food production and livelihoods.
- Environmental Cleanup Costs: Funds spent on pollution control divert resources from productive sectors, hindering economic growth.
What Steps Should Be Taken to Address Pollution in Delhi?
- Congestion Charge: Introducing a congestion charge for private vehicles during peak hours can alleviate traffic congestion and promote public transport or carpooling.
- Revenue generated from this charge can support green projects or subsidize electric vehicles, encouraging eco-friendly choices.
- Cap-and-Trade for Industrial Emissions: Implementing a cap-and-trade system sets emission limits for industries, fostering a market-driven approach to pollution reduction.
- This incentivizes industries to lower emissions and invest in cleaner technologies, ultimately reducing pollution.
- Drones for Pollution Control: Utilizing drones to detect and mitigate pollution hotspots is a proactive measure for managing air quality.
- Drones provide real-time air quality data with high resolution, allowing for public accessibility and targeted intervention.
- Vertical Gardens: Incorporating vertical gardens in urban areas enhances aesthetics and air quality.
- They absorb carbon dioxide, release oxygen, and create habitats for wildlife, contributing to urban biodiversity.
- Rewards for Low-Carbon Lifestyles: Promoting low-carbon living through a rewards system, such as points, vouchers, or tax benefits for eco-friendly choices like public transport or carpooling, encourages environmentally conscious behavior, reducing carbon footprints.
Government Measures to Combat Pollution in Delhi:
- National Clean Air Programme (NCAP): Aims to reduce PM10 and PM2.5 particles by at least 20% by 2024 compared to 2017 levels.
- Graded Response Action Plan (GRAP): As per a Supreme Court order, GRAP outlines actions based on different Air Quality Index categories, addressing air quality in Delhi and the National Capital Region.
- Stubble Burning Mitigation: Various short-term solutions, both in-situ and ex-situ, have been introduced to address crop stubble burning, such as Subsidy to farmers for Turbo happy seeders and bio-decomposers.
- Turbo Happy Seeder (THS) is a machine mounted on a tractor that cuts and uproots the stubble, in order to reduce stubble burning.
- Mobile Enforcement Teams: Enforce regulations against vehicular pollution, complemented by public awareness campaigns and investments in mass rapid transport systems. Phasing out old commercial vehicles is also underway.
- Cleaner Transport: The introduction of BS-VI vehicles, push for electric vehicles (EVs), Odd-Even as an emergency measure and construction of the Eastern and Western Peripheral Expressways to reduce vehicular pollution.
- Improved Farming Practices: Encouraging better disposal of crop residue and exploring cost-effective solutions, like chemical decomposition by the Indian Agricultural Research Institute, are essential for tackling stubble burning.
- "Green War Room": This initiative uses satellite data to identify sources of smog, particularly farm fires in Punjab and Haryana, and takes necessary action.
In response to a growing environmental and health crisis, antipollution measures are being strengthened. However, to ensure success, government bodies at various levels must need to gather the political will to boost investment, foster cross-boundary cooperation, and motivate both citizens and businesses to make their contributions.
Ridding India of Food Insecurity (The Hindu)

- 13 Sep 2023
Why it is in News?
- While India is currently the world's fastest-growing major economy, it is also grappling with a rapid increase in food-price inflation.
- The surge in food prices began to intensify notably in 2019 and has continued to rise in most subsequent years.
- In July of this year, annual inflation surpassed 11%, reaching its highest level in the past decade.
- One consequence of this sustained high food-price inflation is the possibility that a portion of the population may encounter difficulties in accessing food with sufficient nutritional value.
Key Findings of Concern:
- The 'State of Food Security and Nutrition in the World' report by the Food and Agriculture Organization (FAO) assesses the percentage of people in different countries who cannot afford a nutritious diet.
- Approximately 74% of the population is unable to afford a healthy diet.
- This likely results in decreased food consumption due to reduced purchasing power.
- Food prices in India have been on a consistent upward trend since 2019, with annual inflation exceeding 11% in July 2023, the highest rate in a decade.
- There has been a notable increase in the prevalence of anaemia, with over 50% of adult women estimated to be affected according to the latest National Family Health Survey conducted between 2019 and 2021.
- Critics argue that macroeconomic policies, including the Reserve Bank of India's focus on inflation control through measures like inflation targeting, are ineffective in addressing food inflation, which is primarily driven by supply-side factors.
Importance of Food Security:
- Enhanced Health and Nutrition: Food security plays a crucial role in improving the health and well-being of individuals by preventing malnutrition and its associated health issues, including stunted growth, cognitive impairment, and increased susceptibility to diseases.
- It's worth noting that malnutrition is responsible for the deaths of approximately 3.1 million children each year, accounting for nearly half of all child deaths under the age of 5.
- Economic and Social Stability: Food security contributes to the economic and social stability of individuals and nations by enabling increased productivity, income generation, and participation in trade.
- According to a World Bank study, the global cost of undernutrition, in terms of lost productivity and human capital, amounts to USD 3.5 trillion per year.
- Additionally, a United Nations report highlighted that food insecurity played a pivotal role in 58% of conflicts between 2017 and 2019.
- Poverty Alleviation: Food security is instrumental in reducing poverty as it enables people to afford and access nutritious food while also investing in other essential needs such as education and healthcare.
- These factors help break the cycle of poverty.
- National Security: Food security bolsters national security by ensuring a reliable food supply that is not vulnerable to external factors like global food prices or supply chain disruptions.
- Food insecurity can make nations susceptible to such factors, compromising their sovereignty.
- Sustainable Development: Food security aligns with sustainable development goals, particularly Goal 2: Zero Hunger.
- It also supports related goals such as poverty reduction, improved health, gender equality, and environmental sustainability, contributing to a holistic approach to sustainable development.
Causes of Food Insecurity:
- Impact of Russia-Ukraine Conflict: The Russia-Ukraine conflict has disrupted the global supply chain due to trade-related policies imposed by countries, exacerbating the global food crisis.
- Several nations have implemented food trade restrictions to bolster domestic supply and reduce prices.
- Rising Domestic Inflation: Many countries are grappling with domestic food inflation, which has intensified the issue of food insecurity.
- For instance, India has imposed bans on wheat and rice exports to support its domestic population.
- Climate Variability and Extremes: Climate change has significantly affected the availability and quality of critical resources like water, land, and biodiversity essential for food production.
- It has also led to shifts in the patterns and severity of pests, diseases, and natural disasters, resulting in reduced crop yields and livestock productivity.
- The Global Report on Food Crises highlights that weather and climate extremes were the primary drivers of acute food insecurity in 12 countries in 2021, impacting nearly 57 million people.
- Economic Slowdowns and Downturns: Economic slowdowns have diminished the income and job prospects of vulnerable populations, who typically allocate a substantial portion of their income to food purchases.
- These economic shocks have disrupted both the supply and demand for food, leading to increased food prices and reduced food quality.
Learning from the Green Revolution:
- India boasts a rich historical backdrop of the Green Revolution, a transformative period during the 1960s.
- The government initiated a supply-side approach, providing farmers with high-yield seeds, accessible credit, and guaranteed prices through procurement.
- This initiative achieved remarkable success, swiftly liberating India from dependence on food imports and fulfilling its ambition of self-sufficiency.
- However, certain strategic errors were made during this period.
- Excessive use of chemical fertilizers resulted in soil degradation.
- An overemphasis on procurement prices, rather than prioritizing productivity to enhance farm incomes, contributed to inflation.
- The policy primarily focused on cereals, neglecting pulses, a vital source of protein for the majority of Indians.
The Path Ahead: Suggested Actions
- Enhanced Agricultural Investment: Evaluate and optimize public expenditure on irrigation to improve its efficiency.
- Revitalize Research Institutes: Revamp India's network of public agricultural research institutes to rekindle their pivotal role, reminiscent of their contributions during the 1960s.
- Reinvigorate the Role of Local Village Representatives (Gram Sevak): Empower and elevate the role of the gram sevak in villages, making them instrumental in disseminating best agricultural practices.
- Boost Protein-Based Crop Production: Implement a comprehensive program to significantly increase protein production by incorporating various initiatives.
- Foster Cooperative Federalism: Encourage states to actively contribute to enhancing agricultural productivity rather than relying solely on food allocations from the central pool for their Public Distribution System.
- Ensure Permanent Access to a Balanced Diet: Prioritize measures consistent with ecological sustainability to ensure that all Indians have continuous access to a nutritious diet.
- Supply-Side Interventions: Implement interventions on the supply side to stabilize food prices by improving land yield.
- Focus on Cost Reduction: Concentrate on the specific objective of reducing food production costs.
- Multifaceted Approach: Extend irrigation coverage to 100% of the net sown area, eliminate land leasing restrictions, accelerate agricultural research efforts, and reinstate agricultural extension services.
Mains Question:
- Examine the key agricultural issues in India today, encompassing food security, sustainability, and economic stability. Propose a holistic approach that integrates government funding, research, inter-state collaboration, and supply-side interventions to pave the way for a resilient and prosperous future in Indian agriculture. (15M)
India and the Asian Development Bank to establish a climate change and health hub in Delhi (The Hindu)
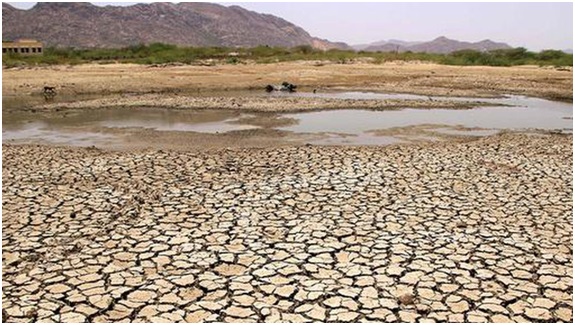
- 28 Aug 2023
Why in the News?
India's G-20 document states that the climate change and health hub will facilitate knowledge sharing, partnerships, and innovations to assist developing countries, while health systems will face challenges from infectious diseases and natural disasters driven by climate change.
Why in the news?
- India, in collaboration with the Asian Development Bank (ADB), is gearing up to inaugurate a climate change and health hub in the national capital.
- This initiative follows India's earlier achievement in hosting the inaugural WHO Centre for Global Traditional Medicine, located in Jamnagar, Gujarat.
- The forthcoming hub's mission is to foster knowledge exchange, cultivate partnerships, drive innovations, and extend support to nations beyond the G-20, with a special focus on developing countries.
The Significance of the Climate Change and Health Hub:
- Fostering Collaboration: This center holds paramount significance as it brings together diverse partners to engage in vital discussions regarding the far-reaching impacts of climate change.
- It provides a unique platform for shared learning and collaboration among stakeholders.
- Addressing Health Emergencies: India's recent G-20 outcome document highlights that climate change remains a key driver of health emergencies, including the resurgence of infectious diseases.
- Moreover, it exacerbates the frequency and severity of natural disasters, posing a significant threat to the capability of health systems to provide essential services.
- Boosting Resilience: Given this backdrop, it is imperative to bolster the resilience of health systems against the adverse effects of climate change.
- The G-20 outcome document outlines a commitment to prioritize the development of climate-resilient health systems, establish sustainable and eco-friendly healthcare supply chains, mobilize resources for resilient, low-carbon health systems, and promote collaboration through initiatives like the WHO-led Alliance for Transformative Action on Climate and Health (ATACH).
- Tackling Zoonotic Spillovers: The recent G-20 Health Ministers' meeting expressed concern about the rising incidence of zoonotic spillovers, leading to the emergence of new diseases.
- In this context, there is an urgent need to identify both new and existing drivers using a scientific and risk-based approach while reinforcing existing infectious disease surveillance systems.
- Global Impact: Situated in New Delhi, the Climate Change and Health Hub is poised to address these pressing issues on a global scale, serving as a hub for international collaboration and solutions.
About Asian Development Bank (ADB):
- Founded in 1966, the Asian Development Bank (ADB) is a multilateral institution that counts 68 members among its ownership, with 49 hailing from the Asian and Pacific region.
- ADB is unwavering in its commitment to fostering a prosperous, inclusive, resilient, and sustainable future for Asia and the Pacific, all while maintaining its steadfast resolve to eliminate extreme poverty.
- To achieve its noble objectives, ADB extends its support to member nations and partners through a comprehensive suite of financial instruments.
- This includes loans, technical assistance, grants, and equity investments, all aimed at catalyzing social and economic development across the region.
- In essence, ADB stands as a stalwart advocate for advancing social and economic development in Asia and the Pacific.
- As of December 31, 2019, ADB's five largest shareholders are Japan and the United States, each possessing 15.6% of total shares, followed by the People's Republic of China (6.4%), India (6.3%), and Australia (5.8%). The institution's headquarters are situated in Manila, Philippines.
About WHO Global Centre for Traditional Medicine (GCTM):
- The WHO Global Centre for Traditional Medicine (GCTM) is a pioneering knowledge hub dedicated to traditional medicine, recognized as the world's premier center of its kind.
- Situated in Jamnagar, Gujarat, it represents a remarkable collaboration between nations.
- India, as the primary investor in GCTM, has committed an approximate sum of US$ 250 million to facilitate the center's establishment, infrastructure development, and operational activities.
The GCTM is designed to achieve five key objectives:
- Archiving Traditional Wisdom: GCTM seeks to harness technology to construct a comprehensive database of traditional knowledge systems.
- Setting International Standards: It aspires to establish global standards for the testing and certification of traditional medicines, enhancing confidence in these age-old remedies.
- Global Knowledge Exchange: The center aims to serve as a global platform where experts in traditional medicine converge to share their experiences and expertise.
- Funding Research: GCTM endeavors to mobilize resources and funding for research in the field of traditional medicines, fostering innovation and scientific exploration.
- Holistic Healing Protocols: The center is dedicated to developing holistic treatment protocols for specific diseases, enabling patients to benefit from the complementary strengths of both traditional and modern medicine approaches.
